Discover how ketamine, a well-established anesthetic, is gaining attention for its medical applications in anesthesia, pain management, and the treatment of psychiatric conditions. Learn about its method of action, interactions in pain pathways, and its use in managing treatment-resistant depression and PTSD. Stay informed about the potential benefits and risks of ketamine and its derivative, esketamine
Ketamine Treatment: A Powerful Option for Pain Management and Mental Health
If you've been dealing with ongoing pain or treatment-resistant depression, you might have heard about ketamine as a possible solution. This medication has been around for decades as an anesthetic, but doctors are now using it in new ways to help people manage chronic pain and certain mental health conditions.
Let's break down what ketamine is, how it works, and whether it might be right for you.
What Is Ketamine?
Ketamine started its medical journey as an anesthetic—a medication that puts you to sleep during surgery. It's been used safely in operating rooms and emergency situations for over 50 years. But here's what's exciting: researchers have discovered that ketamine can do much more than just help during surgery.
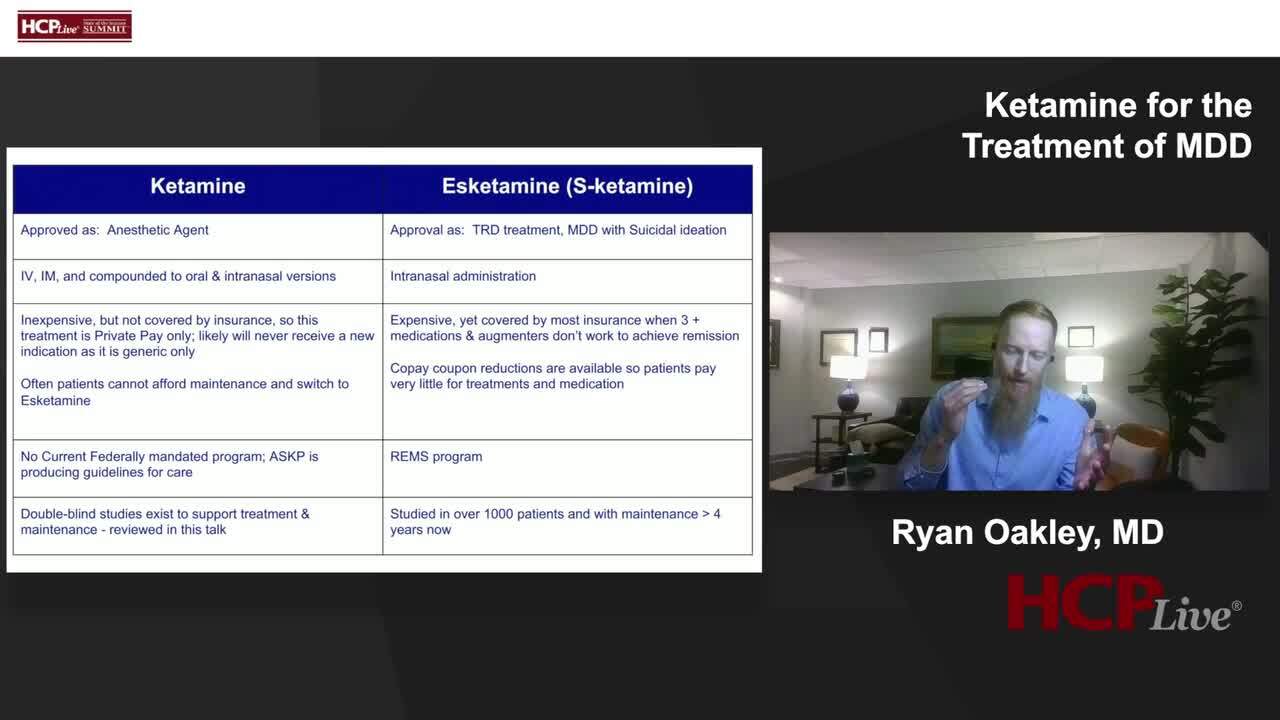
Today, doctors use ketamine treatment for several purposes beyond anesthesia. It's becoming a go-to option for managing both short-term and long-term pain. There's also a version called esketamine (a close relative of ketamine) that the FDA has approved specifically for people with depression that doesn't respond to other treatments and for PTSD.
Think of ketamine as a versatile tool in a doctor's toolkit—one medication with multiple uses depending on what you need.
How Does Ketamine Work in Your Body?
You don't need a medical degree to understand the basics of how ketamine helps with pain. Let's keep it simple.
Your brain has special receivers called NMDA receptors. These receptors are involved in how your brain processes and remembers pain signals. Ketamine blocks these receptors, which is why doctors call it an "NMDA receptor antagonist."
When ketamine blocks these receptors, it affects a brain chemical called glutamate. This chemical plays a big role in sending pain signals throughout your body. By changing how glutamate works, ketamine essentially turns down the volume on your pain signals.
Here's what happens when ketamine goes to work:
It reduces pain sensitivity. Your nervous system becomes less reactive to painful sensations. It's like adjusting the sensitivity settings on your phone—you're still getting the signal, but it's not as intense.
It provides pain relief without being an opioid. This is huge. Ketamine works differently than opioid painkillers, which means it can help you manage pain without the same risk of addiction that comes with medications like oxycodone or morphine.
It works with your brain's natural pain control systems. Ketamine interacts with opioid and dopamine pathways in your brain, making it even more effective at controlling pain.
Using Ketamine for Acute Pain Management
Acute pain is the kind that comes on suddenly—like pain from an injury, surgery, or a medical emergency. Ketamine has proven incredibly useful for managing this type of pain.
Major medical organizations have given ketamine the thumbs up for acute pain management. The American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists all support using intravenous ketamine infusions for short-term pain relief.
What makes ketamine particularly valuable is that it can reduce how much opioid medication patients need. When you're recovering from surgery or dealing with severe injury, combining ketamine with other pain treatments often means you need fewer opioid pills. This lowers your risk of becoming dependent on opioids—a major concern in today's healthcare landscape.
Ketamine Therapy for Chronic Pain
Chronic pain is different from acute pain. It's the kind that sticks around for months or years—pain that becomes part of your daily life. This is where ketamine therapy is showing real promise, though doctors are still learning the best ways to use it.
Research shows that low-dose intravenous ketamine infusions can help people whose pain hasn't responded to other treatments. It's typically used for short-term relief or as part of a bigger treatment plan that includes other therapies.
Conditions That May Benefit from Ketamine Treatment
Medical studies have looked at ketamine for several stubborn pain conditions:
Cancer-related pain. When cancer or cancer treatments cause severe pain that other medications can't control, ketamine may provide relief.
Fibromyalgia. This condition causes widespread pain throughout the body, along with fatigue and sleep problems. Ketamine has shown potential in reducing fibromyalgia pain intensity.
Neuropathic pain. This is pain caused by damaged nerves, often described as burning, shooting, or electric-like sensations. Ketamine can help calm these misfiring nerve signals.
Severe migraines. For people with migraines that don't respond to standard treatments, ketamine infusions might offer relief when nothing else works.
It's important to understand that while these studies look promising, using ketamine for chronic pain is still being researched. Doctors know it can help, but they're still figuring out the best protocols and which patients benefit most.
How Is Ketamine Given?
Ketamine treatment isn't one-size-fits-all. Your doctor will choose the best delivery method based on your specific condition and needs.
Intravenous (IV) infusions are the most common method for pain management. You'll receive ketamine through a small tube inserted into a vein, usually in your arm. The medication drips slowly into your bloodstream over a period of time, typically ranging from 45 minutes to a few hours.
Nasal spray is available for mental health treatment. The FDA-approved esketamine nasal spray is used specifically for treatment-resistant depression and PTSD. You use it under medical supervision at your doctor's office.
Oral medication is another option, though it's less commonly used than IV or nasal forms.
Your doctor will adjust the dose based on how severe your pain is, how you respond to treatment, and whether you have any side effects.
Is Ketamine Safe?
When used properly under medical supervision, ketamine has a solid safety record. Doctors have been using it for decades, so they know a lot about how it affects the body and how to use it safely.
That said, ketamine is classified as a Schedule 3 controlled substance, which means the government regulates it because it has potential for misuse. This is why close monitoring is so important.
Possible Side Effects
Like any medication, ketamine can cause side effects. Most are temporary and manageable, especially when you're being monitored by healthcare professionals:
- Fast heartbeat (tachycardia)
- Blurred vision
- Nausea or upset stomach
- Increased blood pressure (hypertension)
At higher doses, ketamine can cause more intense effects:
- Hallucinations (seeing or hearing things that aren't there)
- Dissociative feelings (feeling disconnected from your body or surroundings, sometimes described as an "out-of-body" experience)
These effects are why medical supervision is crucial. Your healthcare team will watch you closely during treatment and be ready to help if you experience any uncomfortable side effects.
The Rise of Ketamine Clinics: What You Need to Know
In recent years, ketamine clinics have been popping up everywhere. These are private facilities specifically focused on providing ketamine treatment, often for chronic pain and mental health conditions.
This growth is exciting because it means more access to ketamine therapy. However, it also raises some concerns. Not all clinics follow the same rigorous safety standards that hospitals use. There can be significant differences in:
- Staff training and qualifications
- Patient monitoring protocols
- Treatment protocols and dosing
- Follow-up care
Here's what this means for you: If you're considering ketamine treatment at a private clinic, do your homework. Ask about the clinic's safety protocols, the qualifications of the medical staff, and how they monitor patients during and after treatment. A reputable clinic will be happy to answer these questions.
The best ketamine clinics operate with the same high standards you'd find in a hospital setting. They should have:
- Licensed medical professionals overseeing treatment
- Proper monitoring equipment
- Emergency protocols in place
- Clear treatment plans tailored to your specific needs
- Follow-up care and support
FDA Approval: What's Official and What's Off-Label?
Understanding FDA approval helps you know what ketamine is officially cleared for versus where doctors use their professional judgment.
FDA-approved uses:
- As an anesthetic during surgery and medical procedures
- Esketamine nasal spray for treatment-resistant depression and PTSD (approved in 2019)
Off-label use:For chronic pain management, ketamine is used "off-label." This doesn't mean it's experimental or unsafe—it just means doctors are using the medication for a purpose beyond what the FDA originally approved it for. Off-label use is common in medicine and is completely legal when done by qualified healthcare providers following established guidelines.
If your doctor recommends ketamine for chronic pain, they should explain why they think it's appropriate for your situation and discuss the evidence supporting its use.
Is Ketamine Treatment Right for You?
Ketamine isn't typically a first-line treatment. Most doctors consider it when other options haven't worked or as part of a comprehensive pain management strategy.
You might be a candidate for ketamine therapy if:
- You have chronic pain that hasn't responded to other treatments
- You're trying to reduce your reliance on opioid medications
- You have complex pain conditions that affect your quality of life
- Standard pain management approaches haven't given you adequate relief
The best way to determine if ketamine is right for you is to talk with a pain management specialist. These doctors have specific training in complex pain conditions and can evaluate whether ketamine therapy fits into your overall treatment plan.
Working with Your Healthcare Team
If you're considering ketamine treatment, here are some questions to ask your doctor:
- Why do you recommend ketamine for my condition?
- What are the potential benefits and risks in my specific case?
- How will you monitor me during treatment?
- How many treatments will I need?
- What other treatments should I be doing alongside ketamine?
- What happens if ketamine doesn't work for me?
- How will we know if the treatment is working?
Remember, ketamine therapy works best as part of a broader pain management plan. This might include physical therapy, lifestyle changes, psychological support, and other medications or treatments.
The Bottom Line on Ketamine Treatment
Ketamine represents an important option for people dealing with difficult-to-treat pain and certain mental health conditions. Its unique way of working in the brain and body makes it valuable, especially for people who haven't found relief with other approaches.
The key points to remember:
- Ketamine has been used safely in medicine for over 50 years
- It works differently than opioids, offering pain relief without the same addiction risks
- It's FDA-approved as an anesthetic and (in nasal spray form) for treatment-resistant depression and PTSD
- For chronic pain, it's used off-label but supported by medical research and guidelines
- Safety and proper monitoring are essential, whether you're treated in a hospital or clinic
- It's typically considered when other treatments haven't worked
As research continues, we're learning more about how ketamine can help different conditions. The medical community is working to establish even better guidelines and protocols to ensure everyone who might benefit from ketamine treatment can access it safely and effectively.
Take the Next Step Toward Relief
If chronic pain or treatment-resistant depression is affecting your quality of life, it's worth having a conversation with your doctor about ketamine therapy. Don't let pain control your life when new treatment options are available.
Ready to explore your options? Talk to your healthcare provider about whether ketamine treatment might be appropriate for your situation. If you don't have a pain management specialist, ask your primary care doctor for a referral to someone who specializes in complex pain conditions.
You deserve to feel better. With the right medical guidance and proper safety protocols, ketamine treatment could be a valuable tool in your journey toward better pain management and improved quality of life.
Remember: This article is for informational purposes only and doesn't replace professional medical advice. Always consult with qualified healthcare providers about your specific health concerns and treatment options.
Last edited by a moderator: