FunkOdyssey
Seeker of Wisdom
Your comment touches on a very interesting phenomenon with hCG that has puzzled me: hCG monotherapy is capable of producing high physiologic levels of testosterone. It is not uncommon for men to produce 600, 800, 1000 ng/dL or higher testosterone with hCG monotherapy. However, when hCG is added to TRT, you're lucky to get more than a 100 ng/dL bump of total testosterone. Why?One factor that you may not be considering is the impact of trt on leydig cells. If around 20-25% of aromatase in males happens there, then clearly any degradation in the ability of those cells to function would(or at least should I would imagine) impact aromatase abilities.
I dug into it this morning: "There’s credible evidence that exogenous androgen itself directly dampens Leydig-cell steroidogenesis, creating a testis‑level brake that helps explain the small ΔT you see when hCG is layered onto TRT."
and
"Multiple lines show direct, AR‑dependent suppression of Leydig steroidogenic machinery and reduced LHCGR/cAMP signaling capacity with high androgen exposure, alongside classic hCG desensitization biology. That constellation makes it plausible that hCG adds little serum T on top of TRT, while still driving noticeable E2. (ResearchGate, Oxford Academic, PMC, PMC)"
The full story here:
1) Androgen receptor–mediated short-loop feedback inside Leydig cells.
High testosterone activates AR in Leydig cells and represses cAMP‑stimulated steroidogenic genes (e.g., CYP17A1, CYP11A1, STAR) and increases cAMP phosphodiesterases, lowering cAMP signaling efficiency. In rats, pharmacologic T reduced STAR, CYP11A1, CYP17A1, TSPO, SCARB1, and depressed hCG‑stimulated androgen output, while upregulating AR and HSD3B. Direct in‑vitro T reproduced much of this repression, showing a testis‑intrinsic effect, not only pituitary feedback. Reviews also describe this as a Leydig “short feedback loop.” (ResearchGate, Oxford Academic, PMC)
Mechanistic implication: under TRT, Leydig cells are chronically AR‑activated and biased toward lower responsiveness (and toward progesterone→androgen conversion via ↑3β‑HSD), so a modest hCG pulse adds little extra testosterone to the circulation.
2) Gonadotropin receptor/signaling desensitization with sustained stimulation.
Leydig cells show time‑ and dose‑dependent loss of LHCGR (LH/hCG receptor) and downstream signaling after exposure to hCG, with reduced steroidogenic response even to distal cAMP agonists — a classic homologous and postreceptor desensitization. In intact animals and MA‑10 cells this follows hours to days of exposure and then gradually resensitizes. On TRT, endogenous LH is already suppressed; adding intermittent hCG can still cause acute E2/T bursts followed by partial desensitization, limiting additional T output between doses. (PMC)
3) Structural and substrate constraints under LH deprivation.
Chronic LH suppression (as on TRT) shrinks Leydig functional capacity (less SER, cholesterol transport proteins) and drastically lowers intratesticular T (ITT); hCG restores ITT dose‑dependently but you need substantial receptor drive to get back to baseline capacity. In men given 200 mg TE weekly, ITT fell ~94%; 125/250/500 IU hCG qod restored ITT to ~75%, ~93%, and ~126% of baseline, respectively. That rescue of ITT mainly supports spermatogenesis; serum T barely moves because the circulating pool is already dominated by exogenous T. (PubMed)
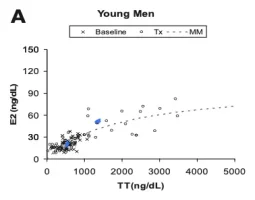
4) Kinetics favor estradiol spikes over large serum T bumps.
After a single hCG dose in men, E2 peaks at ~24 h, whereas serum T peaks ~72 h and is more blunted in men with higher baseline LH (a proxy for impaired Leydig reserve). Under TRT, with Leydig cells partially down‑regulated, you still see ample E2 (Leydig and peripheral aromatase) but only a small serum T increment (~100 ng/dL) because: (a) testicular T output is muted by items 1–3; (b) much of the incremental androgen is aromatized; and (c) the added T is small relative to the exogenous T baseline. (PubMed)
5) Leydig cells are outside the blood–testis barrier.
So systemic androgens (and hCG) can directly reach Leydig cells, consistent with the local AR‑mediated repression observed above. (PMC)
So, to your core question
Is there suppression of Leydig activity in the face of high circulating T? Evidence?
Yes. Multiple lines show direct, AR‑dependent suppression of Leydig steroidogenic machinery and reduced LHCGR/cAMP signaling capacity with high androgen exposure, alongside classic hCG desensitization biology. That constellation makes it plausible that hCG adds little serum T on top of TRT, while still driving noticeable E2. (ResearchGate, Oxford Academic, PMC, PMC)
Caveats (skeptical view)
- Most mechanistic data are rodent or cell‑line; human confirmation is indirect (hCG test kinetics, ITT studies). Still, the directionality is consistent. (PubMed, PubMed)
- The intensity of repression likely depends on TRT dose, trough levels, and time on therapy; intermittent lower‑dose TRT may permit more Leydig responsiveness than steady high levels. (Inference from mechanisms above.) (ResearchGate, PMC)
- Obesity, insulin resistance, leptin, and local cytokines can further blunt Leydig responses independent of TRT. If present, they’d magnify the small ΔT phenomenon. (Oxford Academic, PMC, Oxford Academic)
If you wanted to test the hypothesis clinically
- hCG stimulation while on TRT: measure T, E2 at 0, 24, 72 h after a standardized hCG dose; compare with the same protocol after a TRT washout (if clinically acceptable). Expect larger T AUC off TRT, with earlier/larger E2 peaks in both states. (PubMed)
- Markers of Leydig capacity: 17‑OHP and ITT (if accessible via fine‑needle aspiration) before/after a few weeks of low‑dose hCG on top of TRT; compare to Coviello dosing. (PubMed, PubMed)
- Dose–response: if the goal is fertility/ITT preservation, titrate to the minimal hCG that normalizes ITT or 17‑OHP, accepting that serum T may barely change. (PubMed)