madman
Super Moderator
The testosterone paradox of advanced prostate cancer: mechanistic insights and clinical implications (2022)
Rajendra Kumar, Laura A. Sena, Samuel R. Denmeade & Sushant Kachhap
Abstract
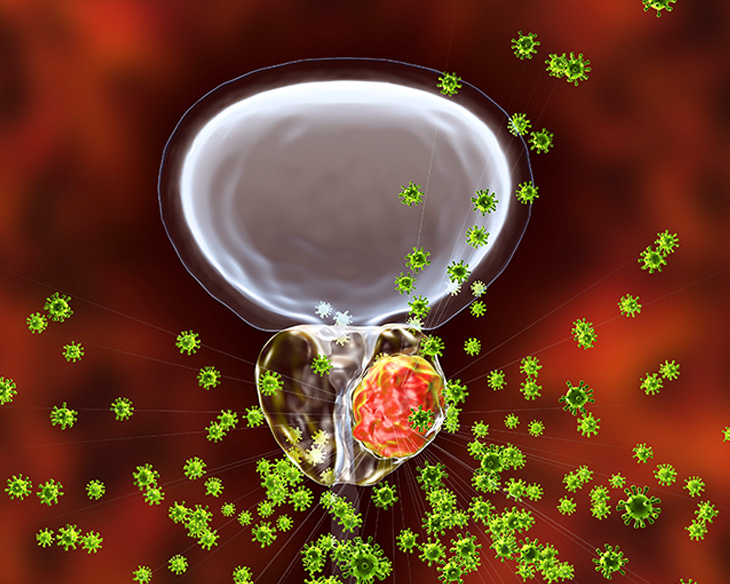
The discovery of the benefits of castration for prostate cancer treatment in 1941 led to androgen deprivation therapy, which remains a mainstay of the treatment of men with advanced prostate cancer. However, as early as this original publication, the inevitable development of castration-resistant prostate cancer was recognized. Resistance first manifests as a sustained rise in the androgen-responsive gene, PSA, consistent with the reactivation of the androgen receptor axis. Evaluation of clinical specimens demonstrates that castration-resistant prostate cancer cells remain addicted to androgen signaling and adapt to chronic low-testosterone states. Paradoxically, the results of several studies have suggested that treatment with supraphysiological levels of testosterone can retard prostate cancer growth. Insights from these studies have been used to investigate the administration of supraphysiological testosterone to patients with prostate cancer for clinical benefits, a strategy that is termed bipolar androgen therapy (BAT). BAT involves rapid cycling from supraphysiological back to near-castration testosterone levels over a 4-week cycle. Understanding how BAT works at the molecular and cellular levels might help to rationalize combining BAT with other agents to achieve increased efficacy and tumor responses.
Introduction
Adenocarcinoma of the prostate gland is the second most common cancer in men, with ~2.2 million new instances and ~375,000 deaths estimated to occur during 2022 (ref. 1).
Androgen signaling has an important role in prostate cancer progression, Androsterone was the first androgen to be isolated from men’s urine2,3. Subsequently, a more potent androgen than androsterone was discovered in the testes, which are a rich source of androgenic hormones, and was termed testosterone from the words testes, sterol, and ketone4. Testosterone is primarily produced by Leydig cells in the testes in response to a luteinizing hormone secreted by the anterior pituitary, and mostly circulates bound to serum hormone-binding globulin5,6 with only the free form gaining entry into cells owing to its lipophilic nature7,8. Upon entry into prostate cells, testosterone is converted to 5 α-dihydrotestosterone (DHT), a highly potent androgen, by the enzyme 5-α reductase9. Testosterone is sufficient for the development of embryonic Wolffian ducts but insufficient for the complete development of prostate and external genitalia, which requires 5-α reductase activity and formation of DHT10,11. Results of early studies showed that radiolabelled DHT or testosterone was selectively retained by the prostate nucleus9,12. These initial observations led to the subsequent identification and cloning of the androgen receptor gene (AR) 8,13,14. AR encodes a 100-kDa protein that shares structural similarities with other steroid hormone nuclear receptors, including the glucocorticoid receptor, progesterone receptor, mineral corticoid receptor, and estrogen receptor15. AR protein can be functionally divided into four domains: the N-terminal activation domain, the central DNA binding domain, the hinge domain, and the C-terminal ligand-binding domain (Fig. 1a). Ligand binding results in dimerization and translocation of AR to the nucleus and subsequent activation or repression of its target genes, such as KLK3, TMPRSS2, and NKX3.1 (ref. 16) (Fig. 1b). Specificity of AR binding to androgen binding sites (ARBS) is determined by chromatin-binding proteins and co-regulators17–20. Androgen signaling is important in the development and progression of all stages of prostate cancer21,22
The role of androgen signaling in prostate cancer progression forms the basis for using androgen deprivation therapy (ADT) as a standard of care for metastatic or recurrent disease23–25. Androgen deprivation is known to provide initial therapeutic benefits, but eventually, all men with prostate cancer develop castration-resistant disease26,27. Intriguingly, high-dose androgens at supraphysiological levels lead to a paradoxical decrease in the growth of some models of prostate cancer through poorly understood mechanisms. Understanding how androgens promote or inhibit the growth of prostate cancer will help to develop effective clinical strategies to inhibit prostate cancer growth and progression. Bipolar androgen therapy (BAT) is an innovative therapeutic strategy in which high doses of testosterone are periodically administered to achieve supraphysiological serum testosterone levels to inhibit prostate tumor growth28
In this Review, the role of androgens in prostate homeostasis and prostate cancer and mechanistic findings of growth inhibition by supraphysiological androgens are described, and insights from the results of prostate cancer clinical trials using supraphysiological testosterone (supraphysiological T) are provided. Finally, the future clinical development of BAT as a therapeutic option against prostate cancer is discussed.
The role of androgens and the AR in the prostate
Accumulated evidence from cellular, molecular and developmental studies indicates that androgens are necessary for the development of the prostate gland, and dysregulated AR signaling aids prostate cancer growth and survival.
Androgens and the AR in prostate homeostasis
The prostate gland consists of branched epithelial ducts made up of a pseudostratified epithelium comprising luminal and basal epithelial cells29,30. The underlying stroma contains fibroblast cells, smooth muscle cells, nerve cells, endothelial cells, immune cells, and rare neuroendocrine cells (Fig. 2).
Androgen signaling in prostate cancer
Unlike non-malignant prostate epithelial cells in which AR is dispensable, cell-autonomous AR signaling fuels prostate cancer growth31,32,46. The modulation of AR signaling through AR amplification21,47, splice variants48,49, AR mutation50–52, co-activator, and co-repressor alteration19,53 in human prostate cancer underscores the importance of AR signaling in prostate cancer.
Clinical utility of reducing AR signaling
Inhibition of AR signaling is the mainstay of the systemic treatment of prostate cancer. Inhibition of AR signaling in patients with prostate cancer can be achieved in three ways: reduction of serum testosterone; inhibition of AR; and degradation of AR. Reduction of serum testosterone can be achieved by blocking its production from the testes and/or adrenal glands63.
The testosterone paradox
Huggins was the first to note that an excess of hormones can cause paradoxical regression of tumours82. His observation was based on the regression of breast tumors upon treatment with a combination of supraphysiological levels of estrogens and progesterone. Huggins called this phenomenon ‘hormone interference’ and noted it as a novel therapeutic approach to treating cancer. To understand the mechanism of this paradoxical effect, the effect of supraphysiological T on prostate cancer cells was tested. Initial studies mainly focused on the effect of supraphysiological T on cell-cycle and cell-death pathways; results of subsequent investigations showed a number of possible mechanisms using both in vitro and in vivo preclinical models; however, the supraphysiological T paradox is not clearly understood.
Testosterone as a drug
In the past decade, in spite of its reputation as a growth factor for prostate cancer, testosterone has been tested as a therapeutic agent for the treatment of this disease.
Early use of testosterone for patients with prostate cancer
Testosterone was initially given to patients with prostate cancer to confirm that the beneficial effect of castration was a result of the reduction of testosterone23. Indeed, many early reports indicated that testosterone administration reversed the benefits of castration, resulting in the elevation of tumor markers that were used at that time (including acid phosphatase and alkaline phosphatase) and symptomatic progression130–132, supporting the role of androgens as growth factors for prostate cancer. Given this observation, androgens were given to patients with the intent of stimulating cancer cell proliferation to sensitize them to subsequent DNA damaging agents, such as radioactive phosphorus (32 P), cyclophosphamide, 5-FU, methotrexate, and doxorubicin133–135; however, the results of these studies were uniformly negative in improving patient outcomes. Yet, scattered among these initial descriptions of testosterone administration for patients with prostate cancer are anecdotal case reports of patients who paradoxically improved with testosterone monotherapy. In 1957, patient HG, a 68-year-old man with metastatic prostate cancer that had progressed following orchiectomy and hypophysectomy, was described as having a dramatic decrease in serum acid phosphatase from near 200 BU/100 cc to undetectable levels and improvement in cancer symptoms following treatment with testosterone propionate. In 1967, patient CJS, a 76-year-old man with ‘preterminal’ metastatic CRPC (mCRPC), was described to improve from an “extremely feeble” state, “unable to sit without assistance,” to “totally pain-free” and “dancing weekly” following treatment with testosterone propionate 100 mg three-times weekly136. Yet these case reports were anti-dogmatic, and further clinical investigation into whether testosterone could be used as a therapy for prostate cancer was slow. Notably, a substantial body of literature describes the use of androgen replacement in men with hypogonadism and prostate cancer. The results of these studies suggest that androgen replacement does not result in rapid prostate cancer disease progression, contrary to the previously widely held view that androgens would rapidly increase prostate cancer growth137–142. They established a precedent that testosterone could be safely administered to patients with prostate cancer, which enabled subsequent studies assessing testosterone as a prostate cancer therapy. Thus, in 2009, two groups reported on the use of transdermal testosterone as a treatment for patients with CRPC143,144. Using transdermal testosterone, physiological levels of serum testosterone of 300–850 ng/dl, which were generally well tolerated, were achieved in both studies. However, the efficacy of this approach was quite modest, with 3 of 15 patients with non-metastatic CRPC demonstrating a decrease in PSA (no patient with >50% decrease) in one study, and only 1 of 12 patients with mCRPC demonstrating a reduction in PSA of 50% in the other study143. Despite this limited efficacy, these studies supported the growing appreciation that testosterone could be administered safely to patients with advanced prostate cancer.
Bipolar androgen therapy
BAT is the administration of testosterone cypionate 400 mg intramuscularly every 28 days concurrent with an LHRH agonist to result in an oscillation of serum testosterone from supraphysiological (>1,500 ng/dl) to near-castration levels145. This therapy was first tested when it was given to 16 patients involved in a pilot clinical trial in combination with etoposide as a treatment for asymptomatic mCRPC145. Remarkably, this combination therapy resulted in PSA and radiographic responses in about half of the patients involved, with 4 patients treated with BAT for >1 year145. The design of this trial was such that patients received BAT and etoposide for the first 3 months, then subsequently received BAT monotherapy if they were experiencing a PSA decline. Notably, most patients who responded to BAT and etoposide continued to respond to BAT monotherapy; thus, etoposide was thought to contribute minimal benefit but considerable toxic effects and was omitted from subsequent trials of BAT.
BAT differs in two important ways from transdermal testosterone administration: first, it achieves supraphysiological levels of serum testosterone; and second, the testosterone level is not clamped but rather is cycled between high and low levels (hence the name ‘bipolar’ androgen therapy)28. This strategy was selected given preclinical data suggesting that CRPC exhibits a biphasic response to re-exposure to androgens, whereby physiological levels of androgens induce growth and proliferation, and supraphysiological levels of androgens are required to induce growth arrest and cell death146. Moreover, this cycled approach was hypothesized to target the heterogeneity and adaptability of prostate cancer cells present in metastases, some of which might be inhibited by high testosterone and others by low testosterone.
Following the promising results of the pilot clinical trial, BAT has been tested in five subsequent clinical trials for patients with advanced prostate cancer: a single-arm trial for castration-sensitive prostate cancer (BATMAN)147; a single-arm, multicohort trial for CRPC (RESTORE)148–150; a randomized trial for mCRPC comparing BAT with enzalutamide (TRANSFORMER)151; a single-arm trial of BAT in combination with the anti-PD1 agent nivolumab for patients with mCRPC (COMBAT)152; and a single-arm, multicohort trial of BAT in combination Following the promising results of the pilot clinical trial, BAT has been tested in five subsequent clinical trials for patients with advanced prostate cancer: a single-arm trial for castration-sensitive prostate cancer (BATMAN)147; a single-arm, multicohort trial for CRPC (RESTORE)148–150; a randomized trial for mCRPC comparing BAT with enzalutamide (TRANSFORMER)151; a single-arm trial of BAT in combination with the anti-PD1 agent nivolumab for patients with mCRPC (COMBAT)152; and a single-arm, multicohort trial of BAT in combination with the poly (ADP-ribose) polymerase (PARP) inhibitor olaparib for mCRPC153. Overall, nearly 300 patients with prostate cancer have been treated with BAT, and a great deal has been learned regarding safety, efficacy, and novel vulnerabilities and opportunities for synergistic combination therapies with BAT, although much remains to be understood.
Safety and tolerability of BAT
Given the efficacy of ADT in treating prostate cancer67, the safety and tolerability of BAT (as the opposite therapy of ADT) have been heavily scrutinized. Evidence from early reports suggested that testosterone can exacerbate pain owing to bone metastases130,134,154,155, and many have voiced concern that testosterone could induce tumor flare that might result in the dangerous spinal cord or urethral compression. Thus, all clinical trials of BAT have excluded patients with pain caused by prostate cancer requiring opiate medications and those with evidence of disease in sites that might put the patient at risk of complications should tumor flare occur. With these exclusion criteria in place, BAT has seemed to be relatively safe and very well-tolerated among treated patients. Overall, the rate and severity of adverse events seem similar to the standard-of-care agent enzalutamide151. Common adverse events tend to be low grade and include musculoskeletal pain, lower extremity edema, and breast tenderness149,151. Notably, spinal cord compression, urethral compression causing urinary obstruction, or other objective evidence of tumor flare have not been observed with the use of BAT. This observation suggests that BAT does not cause tumor flare, but this possibility will be continuously assessed as increased numbers of patients are treated.
Efficacy of BAT monotherapy
The efficacy of BAT monotherapy has been tested in patients with castration-sensitive prostate cancer (BATMAN)147, CRPC that has progressed on only ADT (RESTORE cohort C)149, CRPC that has progressed on abiraterone (RESTORE cohort B and TRANSFORMER)148,151, and CRPC that has progressed on enzalutamide (RESTORE cohort A)150; however, only the TRANSFORMER trial151 was a randomized controlled trial, which means it included a control arm to assess the benefit of this therapy most accurately. On average, among patients with mCRPC, BAT results in a PSA decline ≥50% (PSA50 response) in 20–25% of patients, an objective response in 30–40% of patients, and a median progression-free survival of ~6 months. Efficacy end points studied include the PSA50 response rate (the percentage of patients with at least a 50% decline in PSA on therapy), the objective response rate (ORR) per RECIST 1.1 (ref. 156), and Prostate Cancer Working Group 3 (PCWG3) definitions157, clinical or radiographic progression-free survival PCWG3 definition157 and overall survival (OS) (Table 2).
*Biomarkers for predicting response to BAT
*Sequencing of BAT with AR-axis inhibitory therapies
Opportunities for synergistic combination therapies
BAT is generally well tolerated151. Moreover, in contrast to second-generation AR-axis inhibitors, BAT is associated with minimal financial toxicity and requires no commitment of compliance on behalf of the patient, as it is administered by rapid intramuscular injection monthly in the clinic151. Thus, BAT is an ideal foundation on which to layer additional therapies that might augment responses. Treatments that have been tested in combination with BAT include the anti-PD1 agent nivolumab (COMBAT152) and the PARP inhibitor olaparib153. Outcomes of these clinical trials have been reported currently in abstract form only 152,153.
Future directions
Many questions remain in a quest to define the optimal clinical application of the testosterone paradox in prostate cancer. The optimal schedule and dose of testosterone administration remain to be determined. Results of previous studies indicate that strategies that achieve sustained physiological serum levels of testosterone are not as effective as BAT143,144, which produces cycling of serum testosterone from supraphysiological to near-castration levels over the course of 28 days145; however, whether BAT is more effective simply owing to its ability to expose tumors to increased concentrations of testosterone or whether the cycling of testosterone is important to prevent rapid adaptation of the cancer cells to high levels of testosterone (or both) is currently unknown. One feature of testosterone cypionate is that it has variable pharmacokinetics145. Future clinical studies should consider whether other forms of AR agonists, such as novel formulations of oral testosterone including Jatenzo, an oral lipoprotein-coated testosterone undecanoate, or selective AR modulators, small-molecular non-steroidal AR agonists, might be more or less effective than testosterone cypionate.
Patient factors that predict sensitivity to BAT also need to be determined. Clinical studies of BAT have shown that only 20–40% of patients with CRPC are sensitive to BAT151. Thus, understanding the mechanisms of sensitivity and primary resistance is essential to limiting the use of BAT to only patients who are likely to respond and developing novel strategies to overcome primary resistance to BAT to expand the population of patients who benefit. Promising features that might predict response to BAT include high AR activity158 and homologous recombination repair mutations119, although these biomarkers require prospective validation. A related question is the optimal timing of administration of BAT in the sequence of therapy for patients with CRPC. Current evidence suggests that progression on prolonged and potent AR-axis inhibitors might enhance sensitivity to BAT151; however, BAT priming can improve sensitivity to AR-axis inhibitors149. Thus, future studies should assess the optimal timing of BAT usage for the treatment of patients with advanced prostate cancer.
A challenge is that we have not tested BAT among patients with pain from prostate cancer. An understanding of the molecular mechanisms by which testosterone administration causes or exacerbates pain is needed to broaden the population of patients who might receive and benefit from BAT. Given the usual rapid onset of pain flares, it seems unlikely that this pain is a result of cancer cell proliferation and is more probably a neuromodulatory effect owing to the production of cytokines or other pain-inducing chemical substances, but this idea is currently speculation and future research should directly address this question.
The drivers of acquired resistance to BAT also need to be determined. The majority of patients who initially respond to BAT unfortunately go on to develop resistance at around 6 months to 1 year151. BAT results in considerable downregulation of AR expression158 and this reduction is probably a substantial driver of acquired resistance to therapy. Deciphering this mechanism is important given that this adaptive resistance might be reversible. Alternative mechanisms of resistance should also be considered and studied.
The key mechanisms of tumor growth inhibition by BAT occurring in patients are important to discover. Given the diverse maladaptive effects of supraphysiological androgens in models of prostate cancer158, clinically, several mechanisms probably occur. This knowledge might lead to an understanding of novel vulnerabilities or adaptive responses induced by BAT that could be targeted concurrently with BAT to result in expanded efficacy.
Finally, the cancer cell-extrinsic effects of supraphysiological androgen and BAT that might alter prostate cancer progression need to be understood. Androgens can affect the function of diverse cell types, including immune and stromal cells within the tumor microenvironment167,168, and those of distant tissues such as bone and muscle, which might indirectly affect cancer progression169.
Conclusions
Despite the fundamental function of androgens as growth factors for prostate cancer, preclinical and clinical studies have established that supraphysiological androgens can paradoxically suppress the growth of CRPC. Accumulated preclinical evidence suggests that this growth inhibition can result from multiple mechanisms including cell cycle arrest, senescence, apoptosis, non-apoptotic cell death, and immune clearance. The scientific community has made substantial progress in defining and elucidating mechanisms of the testosterone paradox of advanced prostate cancer, but considerable knowledge still needs to be gained to maximize opportunities for patient benefit. BAT is an innovative approach based on paradoxical growth inhibition of prostate cancer by supraphysiological testosterone; however, it has not been incorporated into standard-of-care practices, given the uncertainty in the optimal use of such therapy. We hope that ongoing research efforts will soon establish a role for this therapy to expand options and improve outcomes for patients with advanced prostate cancer.
Rajendra Kumar, Laura A. Sena, Samuel R. Denmeade & Sushant Kachhap
Abstract
The discovery of the benefits of castration for prostate cancer treatment in 1941 led to androgen deprivation therapy, which remains a mainstay of the treatment of men with advanced prostate cancer. However, as early as this original publication, the inevitable development of castration-resistant prostate cancer was recognized. Resistance first manifests as a sustained rise in the androgen-responsive gene, PSA, consistent with the reactivation of the androgen receptor axis. Evaluation of clinical specimens demonstrates that castration-resistant prostate cancer cells remain addicted to androgen signaling and adapt to chronic low-testosterone states. Paradoxically, the results of several studies have suggested that treatment with supraphysiological levels of testosterone can retard prostate cancer growth. Insights from these studies have been used to investigate the administration of supraphysiological testosterone to patients with prostate cancer for clinical benefits, a strategy that is termed bipolar androgen therapy (BAT). BAT involves rapid cycling from supraphysiological back to near-castration testosterone levels over a 4-week cycle. Understanding how BAT works at the molecular and cellular levels might help to rationalize combining BAT with other agents to achieve increased efficacy and tumor responses.
Introduction
Adenocarcinoma of the prostate gland is the second most common cancer in men, with ~2.2 million new instances and ~375,000 deaths estimated to occur during 2022 (ref. 1).
Androgen signaling has an important role in prostate cancer progression, Androsterone was the first androgen to be isolated from men’s urine2,3. Subsequently, a more potent androgen than androsterone was discovered in the testes, which are a rich source of androgenic hormones, and was termed testosterone from the words testes, sterol, and ketone4. Testosterone is primarily produced by Leydig cells in the testes in response to a luteinizing hormone secreted by the anterior pituitary, and mostly circulates bound to serum hormone-binding globulin5,6 with only the free form gaining entry into cells owing to its lipophilic nature7,8. Upon entry into prostate cells, testosterone is converted to 5 α-dihydrotestosterone (DHT), a highly potent androgen, by the enzyme 5-α reductase9. Testosterone is sufficient for the development of embryonic Wolffian ducts but insufficient for the complete development of prostate and external genitalia, which requires 5-α reductase activity and formation of DHT10,11. Results of early studies showed that radiolabelled DHT or testosterone was selectively retained by the prostate nucleus9,12. These initial observations led to the subsequent identification and cloning of the androgen receptor gene (AR) 8,13,14. AR encodes a 100-kDa protein that shares structural similarities with other steroid hormone nuclear receptors, including the glucocorticoid receptor, progesterone receptor, mineral corticoid receptor, and estrogen receptor15. AR protein can be functionally divided into four domains: the N-terminal activation domain, the central DNA binding domain, the hinge domain, and the C-terminal ligand-binding domain (Fig. 1a). Ligand binding results in dimerization and translocation of AR to the nucleus and subsequent activation or repression of its target genes, such as KLK3, TMPRSS2, and NKX3.1 (ref. 16) (Fig. 1b). Specificity of AR binding to androgen binding sites (ARBS) is determined by chromatin-binding proteins and co-regulators17–20. Androgen signaling is important in the development and progression of all stages of prostate cancer21,22
The role of androgen signaling in prostate cancer progression forms the basis for using androgen deprivation therapy (ADT) as a standard of care for metastatic or recurrent disease23–25. Androgen deprivation is known to provide initial therapeutic benefits, but eventually, all men with prostate cancer develop castration-resistant disease26,27. Intriguingly, high-dose androgens at supraphysiological levels lead to a paradoxical decrease in the growth of some models of prostate cancer through poorly understood mechanisms. Understanding how androgens promote or inhibit the growth of prostate cancer will help to develop effective clinical strategies to inhibit prostate cancer growth and progression. Bipolar androgen therapy (BAT) is an innovative therapeutic strategy in which high doses of testosterone are periodically administered to achieve supraphysiological serum testosterone levels to inhibit prostate tumor growth28
In this Review, the role of androgens in prostate homeostasis and prostate cancer and mechanistic findings of growth inhibition by supraphysiological androgens are described, and insights from the results of prostate cancer clinical trials using supraphysiological testosterone (supraphysiological T) are provided. Finally, the future clinical development of BAT as a therapeutic option against prostate cancer is discussed.
The role of androgens and the AR in the prostate
Accumulated evidence from cellular, molecular and developmental studies indicates that androgens are necessary for the development of the prostate gland, and dysregulated AR signaling aids prostate cancer growth and survival.
Androgens and the AR in prostate homeostasis
The prostate gland consists of branched epithelial ducts made up of a pseudostratified epithelium comprising luminal and basal epithelial cells29,30. The underlying stroma contains fibroblast cells, smooth muscle cells, nerve cells, endothelial cells, immune cells, and rare neuroendocrine cells (Fig. 2).
Androgen signaling in prostate cancer
Unlike non-malignant prostate epithelial cells in which AR is dispensable, cell-autonomous AR signaling fuels prostate cancer growth31,32,46. The modulation of AR signaling through AR amplification21,47, splice variants48,49, AR mutation50–52, co-activator, and co-repressor alteration19,53 in human prostate cancer underscores the importance of AR signaling in prostate cancer.
Clinical utility of reducing AR signaling
Inhibition of AR signaling is the mainstay of the systemic treatment of prostate cancer. Inhibition of AR signaling in patients with prostate cancer can be achieved in three ways: reduction of serum testosterone; inhibition of AR; and degradation of AR. Reduction of serum testosterone can be achieved by blocking its production from the testes and/or adrenal glands63.
The testosterone paradox
Huggins was the first to note that an excess of hormones can cause paradoxical regression of tumours82. His observation was based on the regression of breast tumors upon treatment with a combination of supraphysiological levels of estrogens and progesterone. Huggins called this phenomenon ‘hormone interference’ and noted it as a novel therapeutic approach to treating cancer. To understand the mechanism of this paradoxical effect, the effect of supraphysiological T on prostate cancer cells was tested. Initial studies mainly focused on the effect of supraphysiological T on cell-cycle and cell-death pathways; results of subsequent investigations showed a number of possible mechanisms using both in vitro and in vivo preclinical models; however, the supraphysiological T paradox is not clearly understood.
Testosterone as a drug
In the past decade, in spite of its reputation as a growth factor for prostate cancer, testosterone has been tested as a therapeutic agent for the treatment of this disease.
Early use of testosterone for patients with prostate cancer
Testosterone was initially given to patients with prostate cancer to confirm that the beneficial effect of castration was a result of the reduction of testosterone23. Indeed, many early reports indicated that testosterone administration reversed the benefits of castration, resulting in the elevation of tumor markers that were used at that time (including acid phosphatase and alkaline phosphatase) and symptomatic progression130–132, supporting the role of androgens as growth factors for prostate cancer. Given this observation, androgens were given to patients with the intent of stimulating cancer cell proliferation to sensitize them to subsequent DNA damaging agents, such as radioactive phosphorus (32 P), cyclophosphamide, 5-FU, methotrexate, and doxorubicin133–135; however, the results of these studies were uniformly negative in improving patient outcomes. Yet, scattered among these initial descriptions of testosterone administration for patients with prostate cancer are anecdotal case reports of patients who paradoxically improved with testosterone monotherapy. In 1957, patient HG, a 68-year-old man with metastatic prostate cancer that had progressed following orchiectomy and hypophysectomy, was described as having a dramatic decrease in serum acid phosphatase from near 200 BU/100 cc to undetectable levels and improvement in cancer symptoms following treatment with testosterone propionate. In 1967, patient CJS, a 76-year-old man with ‘preterminal’ metastatic CRPC (mCRPC), was described to improve from an “extremely feeble” state, “unable to sit without assistance,” to “totally pain-free” and “dancing weekly” following treatment with testosterone propionate 100 mg three-times weekly136. Yet these case reports were anti-dogmatic, and further clinical investigation into whether testosterone could be used as a therapy for prostate cancer was slow. Notably, a substantial body of literature describes the use of androgen replacement in men with hypogonadism and prostate cancer. The results of these studies suggest that androgen replacement does not result in rapid prostate cancer disease progression, contrary to the previously widely held view that androgens would rapidly increase prostate cancer growth137–142. They established a precedent that testosterone could be safely administered to patients with prostate cancer, which enabled subsequent studies assessing testosterone as a prostate cancer therapy. Thus, in 2009, two groups reported on the use of transdermal testosterone as a treatment for patients with CRPC143,144. Using transdermal testosterone, physiological levels of serum testosterone of 300–850 ng/dl, which were generally well tolerated, were achieved in both studies. However, the efficacy of this approach was quite modest, with 3 of 15 patients with non-metastatic CRPC demonstrating a decrease in PSA (no patient with >50% decrease) in one study, and only 1 of 12 patients with mCRPC demonstrating a reduction in PSA of 50% in the other study143. Despite this limited efficacy, these studies supported the growing appreciation that testosterone could be administered safely to patients with advanced prostate cancer.
Bipolar androgen therapy
BAT is the administration of testosterone cypionate 400 mg intramuscularly every 28 days concurrent with an LHRH agonist to result in an oscillation of serum testosterone from supraphysiological (>1,500 ng/dl) to near-castration levels145. This therapy was first tested when it was given to 16 patients involved in a pilot clinical trial in combination with etoposide as a treatment for asymptomatic mCRPC145. Remarkably, this combination therapy resulted in PSA and radiographic responses in about half of the patients involved, with 4 patients treated with BAT for >1 year145. The design of this trial was such that patients received BAT and etoposide for the first 3 months, then subsequently received BAT monotherapy if they were experiencing a PSA decline. Notably, most patients who responded to BAT and etoposide continued to respond to BAT monotherapy; thus, etoposide was thought to contribute minimal benefit but considerable toxic effects and was omitted from subsequent trials of BAT.
BAT differs in two important ways from transdermal testosterone administration: first, it achieves supraphysiological levels of serum testosterone; and second, the testosterone level is not clamped but rather is cycled between high and low levels (hence the name ‘bipolar’ androgen therapy)28. This strategy was selected given preclinical data suggesting that CRPC exhibits a biphasic response to re-exposure to androgens, whereby physiological levels of androgens induce growth and proliferation, and supraphysiological levels of androgens are required to induce growth arrest and cell death146. Moreover, this cycled approach was hypothesized to target the heterogeneity and adaptability of prostate cancer cells present in metastases, some of which might be inhibited by high testosterone and others by low testosterone.
Following the promising results of the pilot clinical trial, BAT has been tested in five subsequent clinical trials for patients with advanced prostate cancer: a single-arm trial for castration-sensitive prostate cancer (BATMAN)147; a single-arm, multicohort trial for CRPC (RESTORE)148–150; a randomized trial for mCRPC comparing BAT with enzalutamide (TRANSFORMER)151; a single-arm trial of BAT in combination with the anti-PD1 agent nivolumab for patients with mCRPC (COMBAT)152; and a single-arm, multicohort trial of BAT in combination Following the promising results of the pilot clinical trial, BAT has been tested in five subsequent clinical trials for patients with advanced prostate cancer: a single-arm trial for castration-sensitive prostate cancer (BATMAN)147; a single-arm, multicohort trial for CRPC (RESTORE)148–150; a randomized trial for mCRPC comparing BAT with enzalutamide (TRANSFORMER)151; a single-arm trial of BAT in combination with the anti-PD1 agent nivolumab for patients with mCRPC (COMBAT)152; and a single-arm, multicohort trial of BAT in combination with the poly (ADP-ribose) polymerase (PARP) inhibitor olaparib for mCRPC153. Overall, nearly 300 patients with prostate cancer have been treated with BAT, and a great deal has been learned regarding safety, efficacy, and novel vulnerabilities and opportunities for synergistic combination therapies with BAT, although much remains to be understood.
Safety and tolerability of BAT
Given the efficacy of ADT in treating prostate cancer67, the safety and tolerability of BAT (as the opposite therapy of ADT) have been heavily scrutinized. Evidence from early reports suggested that testosterone can exacerbate pain owing to bone metastases130,134,154,155, and many have voiced concern that testosterone could induce tumor flare that might result in the dangerous spinal cord or urethral compression. Thus, all clinical trials of BAT have excluded patients with pain caused by prostate cancer requiring opiate medications and those with evidence of disease in sites that might put the patient at risk of complications should tumor flare occur. With these exclusion criteria in place, BAT has seemed to be relatively safe and very well-tolerated among treated patients. Overall, the rate and severity of adverse events seem similar to the standard-of-care agent enzalutamide151. Common adverse events tend to be low grade and include musculoskeletal pain, lower extremity edema, and breast tenderness149,151. Notably, spinal cord compression, urethral compression causing urinary obstruction, or other objective evidence of tumor flare have not been observed with the use of BAT. This observation suggests that BAT does not cause tumor flare, but this possibility will be continuously assessed as increased numbers of patients are treated.
Efficacy of BAT monotherapy
The efficacy of BAT monotherapy has been tested in patients with castration-sensitive prostate cancer (BATMAN)147, CRPC that has progressed on only ADT (RESTORE cohort C)149, CRPC that has progressed on abiraterone (RESTORE cohort B and TRANSFORMER)148,151, and CRPC that has progressed on enzalutamide (RESTORE cohort A)150; however, only the TRANSFORMER trial151 was a randomized controlled trial, which means it included a control arm to assess the benefit of this therapy most accurately. On average, among patients with mCRPC, BAT results in a PSA decline ≥50% (PSA50 response) in 20–25% of patients, an objective response in 30–40% of patients, and a median progression-free survival of ~6 months. Efficacy end points studied include the PSA50 response rate (the percentage of patients with at least a 50% decline in PSA on therapy), the objective response rate (ORR) per RECIST 1.1 (ref. 156), and Prostate Cancer Working Group 3 (PCWG3) definitions157, clinical or radiographic progression-free survival PCWG3 definition157 and overall survival (OS) (Table 2).
*Biomarkers for predicting response to BAT
*Sequencing of BAT with AR-axis inhibitory therapies
Opportunities for synergistic combination therapies
BAT is generally well tolerated151. Moreover, in contrast to second-generation AR-axis inhibitors, BAT is associated with minimal financial toxicity and requires no commitment of compliance on behalf of the patient, as it is administered by rapid intramuscular injection monthly in the clinic151. Thus, BAT is an ideal foundation on which to layer additional therapies that might augment responses. Treatments that have been tested in combination with BAT include the anti-PD1 agent nivolumab (COMBAT152) and the PARP inhibitor olaparib153. Outcomes of these clinical trials have been reported currently in abstract form only 152,153.
Future directions
Many questions remain in a quest to define the optimal clinical application of the testosterone paradox in prostate cancer. The optimal schedule and dose of testosterone administration remain to be determined. Results of previous studies indicate that strategies that achieve sustained physiological serum levels of testosterone are not as effective as BAT143,144, which produces cycling of serum testosterone from supraphysiological to near-castration levels over the course of 28 days145; however, whether BAT is more effective simply owing to its ability to expose tumors to increased concentrations of testosterone or whether the cycling of testosterone is important to prevent rapid adaptation of the cancer cells to high levels of testosterone (or both) is currently unknown. One feature of testosterone cypionate is that it has variable pharmacokinetics145. Future clinical studies should consider whether other forms of AR agonists, such as novel formulations of oral testosterone including Jatenzo, an oral lipoprotein-coated testosterone undecanoate, or selective AR modulators, small-molecular non-steroidal AR agonists, might be more or less effective than testosterone cypionate.
Patient factors that predict sensitivity to BAT also need to be determined. Clinical studies of BAT have shown that only 20–40% of patients with CRPC are sensitive to BAT151. Thus, understanding the mechanisms of sensitivity and primary resistance is essential to limiting the use of BAT to only patients who are likely to respond and developing novel strategies to overcome primary resistance to BAT to expand the population of patients who benefit. Promising features that might predict response to BAT include high AR activity158 and homologous recombination repair mutations119, although these biomarkers require prospective validation. A related question is the optimal timing of administration of BAT in the sequence of therapy for patients with CRPC. Current evidence suggests that progression on prolonged and potent AR-axis inhibitors might enhance sensitivity to BAT151; however, BAT priming can improve sensitivity to AR-axis inhibitors149. Thus, future studies should assess the optimal timing of BAT usage for the treatment of patients with advanced prostate cancer.
A challenge is that we have not tested BAT among patients with pain from prostate cancer. An understanding of the molecular mechanisms by which testosterone administration causes or exacerbates pain is needed to broaden the population of patients who might receive and benefit from BAT. Given the usual rapid onset of pain flares, it seems unlikely that this pain is a result of cancer cell proliferation and is more probably a neuromodulatory effect owing to the production of cytokines or other pain-inducing chemical substances, but this idea is currently speculation and future research should directly address this question.
The drivers of acquired resistance to BAT also need to be determined. The majority of patients who initially respond to BAT unfortunately go on to develop resistance at around 6 months to 1 year151. BAT results in considerable downregulation of AR expression158 and this reduction is probably a substantial driver of acquired resistance to therapy. Deciphering this mechanism is important given that this adaptive resistance might be reversible. Alternative mechanisms of resistance should also be considered and studied.
The key mechanisms of tumor growth inhibition by BAT occurring in patients are important to discover. Given the diverse maladaptive effects of supraphysiological androgens in models of prostate cancer158, clinically, several mechanisms probably occur. This knowledge might lead to an understanding of novel vulnerabilities or adaptive responses induced by BAT that could be targeted concurrently with BAT to result in expanded efficacy.
Finally, the cancer cell-extrinsic effects of supraphysiological androgen and BAT that might alter prostate cancer progression need to be understood. Androgens can affect the function of diverse cell types, including immune and stromal cells within the tumor microenvironment167,168, and those of distant tissues such as bone and muscle, which might indirectly affect cancer progression169.
Conclusions
Despite the fundamental function of androgens as growth factors for prostate cancer, preclinical and clinical studies have established that supraphysiological androgens can paradoxically suppress the growth of CRPC. Accumulated preclinical evidence suggests that this growth inhibition can result from multiple mechanisms including cell cycle arrest, senescence, apoptosis, non-apoptotic cell death, and immune clearance. The scientific community has made substantial progress in defining and elucidating mechanisms of the testosterone paradox of advanced prostate cancer, but considerable knowledge still needs to be gained to maximize opportunities for patient benefit. BAT is an innovative approach based on paradoxical growth inhibition of prostate cancer by supraphysiological testosterone; however, it has not been incorporated into standard-of-care practices, given the uncertainty in the optimal use of such therapy. We hope that ongoing research efforts will soon establish a role for this therapy to expand options and improve outcomes for patients with advanced prostate cancer.