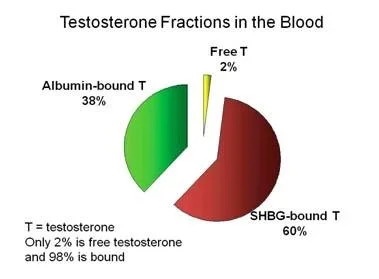
what is the typical % ranges for SHBG and albumin in regards to testosterone fractions in the blood?
The image is one examaple but Every source I come accross says a different thing. We know that 98% is bound. 2% is free... of course the amount bound (SHBG/albumin) is going to be user specific dependent on many factors....but what would be typical % range for the average healthy man?
some sources say 45% SHBG and 53-55% albumin. Others have SHBG as high as 60-70% so what’s typical...
@Nelson Vergel
Many thanks.
E. Nieschlag (2012)
2.1 Introduction
Androgens are essential for the development and function of male reproductive organs, for example, maturation of secondary sexual characteristics, libido, and stimulation of spermatogenesis. Beyond that, androgens influence many somatic organ functions, which are covered in various chapters in this volume. In fact, a large number of organs express androgen receptors (Dankbar et al. 1995).
Physiological effects of androgens depend on different factors such as the number of androgen molecules, distribution of androgens and their metabolites inside the cell, interaction with the receptors, polyglutamine number of the amino-acid sequence in the androgen receptor, and receptor activation (Palazzolo et al. 2008). In order to achieve sufficient exposure to androgens in target tissues, their peripheral and local levels must be well balanced and the transport mechanisms must be in place.
Obviously, production and clearance/excretion rates must be in balance as well. The action of androgens in target cells depends on the amount of steroid which can penetrate into the cells, the extent of metabolic conversions within the cells, the interactions with the receptor proteins, and, finally, upon the action of the androgen receptors at the genomic level. Unless mentioned specifically, this chapter refers to human data. It provides a timely overview of this topic and focuses on Leydig cells, regulation of Leydig cell function, steroidogenesis, transport and metabolism of testosterone, and genomic/non-genomic androgen actions. For more detailed and extensive descriptions on the various topics, the reader may also find the book The Leydig Cell in Health and Disease edited by Payne and Hardy (2007) useful.
2.4 Testosterone transport
During transport in plasma, testosterone is mainly bound to albumin or to SHBG which is produced by hepatocytes. Androgen-binding protein, with similar steroid-binding characteristics when compared to SHBG is produced by Sertoli cells in the testis and is a b-globulin consisting of different protein subunits. In rats, SHBG is expressed in Sertoli cells, secreted preferentially into the seminiferous tubules, and migrates into the caput epididymidis where it is internalized by epithelial cells and modulates androgen-dependent sperm maturation. Testicular SHBG isoforms are found in sperm and released from sperm during the capacitation reaction. Plasma SHBG has about 95 kDa molecular weight, 30% of which is represented by carbohydrates, and possesses one androgen binding site per molecule. Human testicular SHBG transcripts are expressed in germ cells and contain an alternative exon 1 sequence, appearing to encode an SHBG isoform that is 4–5 kDa smaller than plasma SHBG. The testosterone binding capacity is also much lower compared to the plasma SHBG (Selva et al. 2005).
In normal men, only 2% of total testosterone circulates freely in the blood, while 44% is bound to SHBG and 54% to albumin. The binding affinity of testosterone to albumin is about 100 times lower compared to SHBG. However, since albumin concentration is far higher than that of SHBG, the binding capacity of both proteins for testosterone is approximately the same. The ratio of testosterone bound to SHBG over free SHBG is proportional to SHBG concentration. Direct measurement of free testosterone is impractical in routine practice so that several equations are used to estimate the free testosterone concentration in serum (see Chapter 4).
Apparently, the dissociation of testosterone from binding proteins takes place predominantly in capillaries. The interaction of binding proteins with the endothelial glycocalyx leads to a structural modification of the hormonal binding site and thereby to a change in affinity.
As a result, testosterone is set free and can diffuse freely into the target cell, or binds together with SHBG to megalin (Fig. 2.5), a cell importer protein (Hammes et al. 2005). Megalin is expressed in sex-steroid target tissues and is a member of the LDL receptor superfamily of endocytotic proteins.
In the serum, 98–99.5% of the sex steroids are protein-bound, and endocytosis is quantitatively more relevant for tissue delivery of biologically active steroid hormones than free diffusion. To date several different ways have been described by which steroids can enter the target cells, and which of these are the most relevant pathways to take up the various steroid hormones is still being debated.
Sex hormone-binding globulin binds not only testosterone but also estradiol. The type of binding is influenced by the different SHBG isoforms, but generally, testosterone binds threefold higher than estradiol to SHBG. For example, it could be demonstrated that post-translational changes in the carbohydrate structure of SHBG can lead to different binding the affinity of the protein to testosterone or estradiol.
Sex hormone-binding globulin concentration in serum is under hormonal regulation and primarily regulated through opposing actions of sex steroids on hepatocytes: estrogen stimulates and androgen inhibits SHBG production. Other hormones such as the thyroid hormones are also potent stimulators of SHBG production. Sex hormone-binding globulin concentration in men is about one-third to one-half of the concentration found in women.
*In normal, healthy men with an intact hypothalamic-pituitary-testicular axis, an increase in plasma concentrations of SHBG leads to an acute decrease of free testosterone and simultaneous stimulation of testosterone synthesis, persisting until the achievement of normal concentrations.
Testosterone concentrations in the testicular lymphatic circulation and in the venous blood are very similar, but there are essential differences in the flow rate and velocity of both systems.
Therefore transport of testosterone in the general blood circulation occurs mainly through the spermatic vein. Androgens diffuse into interstitial fluid and then enter testicular capillaries or enter capillaries directly from Leydig cells that are in direct contact with the testicular microvasculature. The mechanism for testosterone transport from the Leydig cell into the blood or lymph is not completely known. Probably lipophilic steroids distributed within cells or small cell groups are released through passive diffusion. On the other hand, mouse studies have raised the possibility of an active testosterone transport being important for spermatogenesis (Takamiya et al. 1998), showing that gangliosides-associated testosterone transport appeared necessary for complete spermatogenesis.
Steroids such as pregnenolone, progesterone, and testosterone not only rapidly pass the Leydig cell membranes, but they can also equilibrate rapidly between different testicular compartments, and the testicular secretion pattern is most likely determined by amounts that are produced inside the tissue, the permeability characteristics of the membranes and the binding proteins in various testicular fluids (Rommerts 2004). As the blood flow is much higher than the flow of interstitial fluid, most of the unconjugated steroids diffuse from the interstitial space to the blood and leave the testis via venous blood.
Estradiol is produced by Leydig cells, but the amount is small, with about 20% of peripheral aromatization (Rommerts 2004).
Fig. 2.6 Quantitative aspects of production, transport, and metabolism of biologically active androgens. The majority of testosterone is derived from the testis. During peripheral transport, most of the testosterone is bound to transport proteins. In peripheral tissues, testosterone is either metabolized or converted into other active steroids such as DHT or estradiol. Based upon Rommerts (2004).
4.2 Testosterone, dihydrotestosterone, and sex hormone-binding globulin in blood
Testosterone and DHT circulate in serum largely bound to transport proteins: that is albumin, which displays low affinity but very high binding capacity, and SHBG, with high affinity and low capacity. A systematic analysis of serum transport of steroid hormones and their interaction with binding proteins revealed an association constant of SHBG of 1.6 109 M 1 for testosterone and of 5.5 109 M 1 for DHT at 37 C (Dunn et al. 1981). By comparison, the association constant of albumin for testosterone is five orders of magnitude lower (6 104 M 1 ) (Anderson 1974).
The relative amounts of protein binding of circulating testosterone in men and women are shown in Table 4.1.
Table 4.1 Transport of endogenous testosterone and DHT in male and female serum
About 1.5–2% of serum testosterone is free and is believed to represent bioactive testosterone. Free and protein-bound testosterone and DHT are in equilibrium so that when the free hormone is subtracted from circulation because of entry into the tissue, new testosterone dissociates from albumin and SHBG, a new equilibrium is promptly reached, and the free-hormone concentration in serum remains constant. Conversely, pathophysiological conditions causing changes in binding protein concentration (e.g. pregnancy, hypo or hyperthyroidism, growth hormone (GH) excess, treatment with antiepileptic drugs) or displacement of testosterone from SHBG by drugs (e.g. danazol) results in changes in total testosterone concentration in order to maintain constant free testosterone levels.
--------------------------------------------------------------------------------------------------
A multi-step, dynamic allosteric model of testosterone’s binding to sex hormone-binding globulin (2015)
The new dynamic model (Model F) leads us to reconsider several dogmas related to testosterone’s binding to SHBG and have important physiologic and clinical implications.
*First, the fraction of circulating testosterone, which is free is substantially greater (2.9 ± 0.4%) than has been generally assumed (%cFTV 1.5 ± 0.4%).
*Second, percent FT is not significantly related to total testosterone over a wide range of total testosterone concentrations. However, the percent FT declines as SHBG concentrations increase, although it does not decline as precipitously as predicted by Vermeulen’s model. Due to the allostery between the two binding sites, SHBG is able to regulate FT levels in a much larger dynamic range.
5. Conclusions
In summary, experimental data generated using several independent methods provide evidence of an allosteric mechanism of testosterone binding to SHBG dimer. FT concentrations derived using the new dynamic model incorporating multistep interaction with allostery does not differ significantly from those measured using equilibrium dialysis in men and significantly reduces the systematic deviation in cFT values in women. The application of the new model to clinical trial data has revealed new insights into the percent of circulating testosterone that is free, the relation between percent FT and total testosterone and SHBG. The use of additional experimental models, including dimerization-deficient SHBG mutants would allow further insights into molecular mechanisms of testosterone’s interaction with SHBG. The extension of the new dynamic model incorporating allostery should also be further explored in clinical populations as its availability on desktops and mobile devices can provide a convenient and accurate approach for determining FT at the point-of-care, and facilitating the diagnosis and treatment of men and women with androgen disorders.
--------------------------------------------------------------------------------------------------
Keep in mind that although TT is important to know FT is what truly matters as it is the active unbound fraction of testosterone responsible for the beneficial effects.
FT (cFTZ) 16-31 ng/dL would be considered a healthy range.
FT 5-10 ng/dL would be considered low.
An average healthy young male would have calculated FT (cFTZ) in the 16-20 ng/dL range.
Most men on trt will do well with a cFTZ 20-30 ng/dL range.
When testing FT it is critical that you use the most accurate assays such as the gold standard Equilibrium Dialysis or Ultrafiltration if you want to know where your FT truly sits.
Either assay will suffice when it comes to testing FT!
Quest Diagnostics: TT (LC/MS-MS) and FT (ED or UF)
1.
Testosterone, Total and Free (NO Upper Limit) plus Hematocrit
2.
Testosterone, Total, LC/MS, and Free (Equilibrium Ultrafiltration)
Labcorp: TT (LC/MS-MS) and FT (ED or UF)
1.
500726: Testosterone, Free, Mass Spectrometry/Equilibrium Dialysis (Endocrine Sciences) | Labcorp
2.
070038: Testosterone, Free, Equilibrium Ultrafiltration With Total Testosterone, LC/MS-MS | Labcorp