The company that makes Aveed (Nebido outside the US) requires doctors to be registered with them for doctors to prescribe it.
This requirement exists because of the
REMS (Risk Evaluation and Mitigation Strategy) program mandated by the FDA for Aveed.
The core concern: Pulmonary Oil Microembolism (POME)
Aveed's formulation—testosterone undecanoate in castor oil—carries a specific risk of POME, a rare but serious reaction that can occur during or immediately after injection. Symptoms include coughing, shortness of breath, chest tightness, dizziness, and fainting. There's also a risk of anaphylaxis.
What the REMS requires:
- Healthcare setting certification — Aveed can only be administered in a certified healthcare setting (not at home), where staff are trained to recognize and manage POME and anaphylactic reactions
- Prescriber enrollment — Doctors must register with the Aveed REMS program, confirming they understand the risks and will only prescribe it for administration in appropriate settings
- Post-injection observation — Patients must be monitored for 30 minutes after each injection
Why this differs from other testosterone formulations:
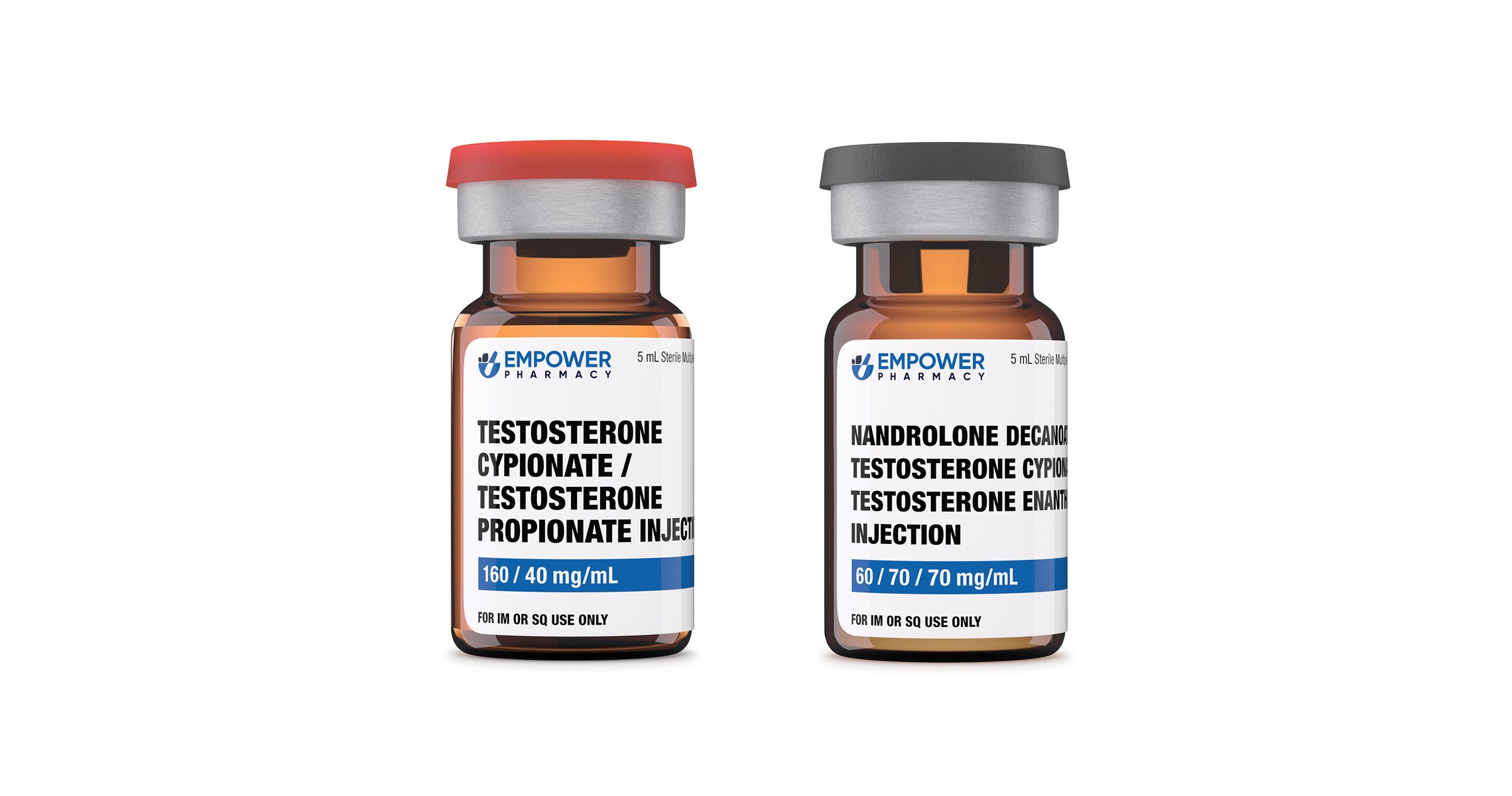
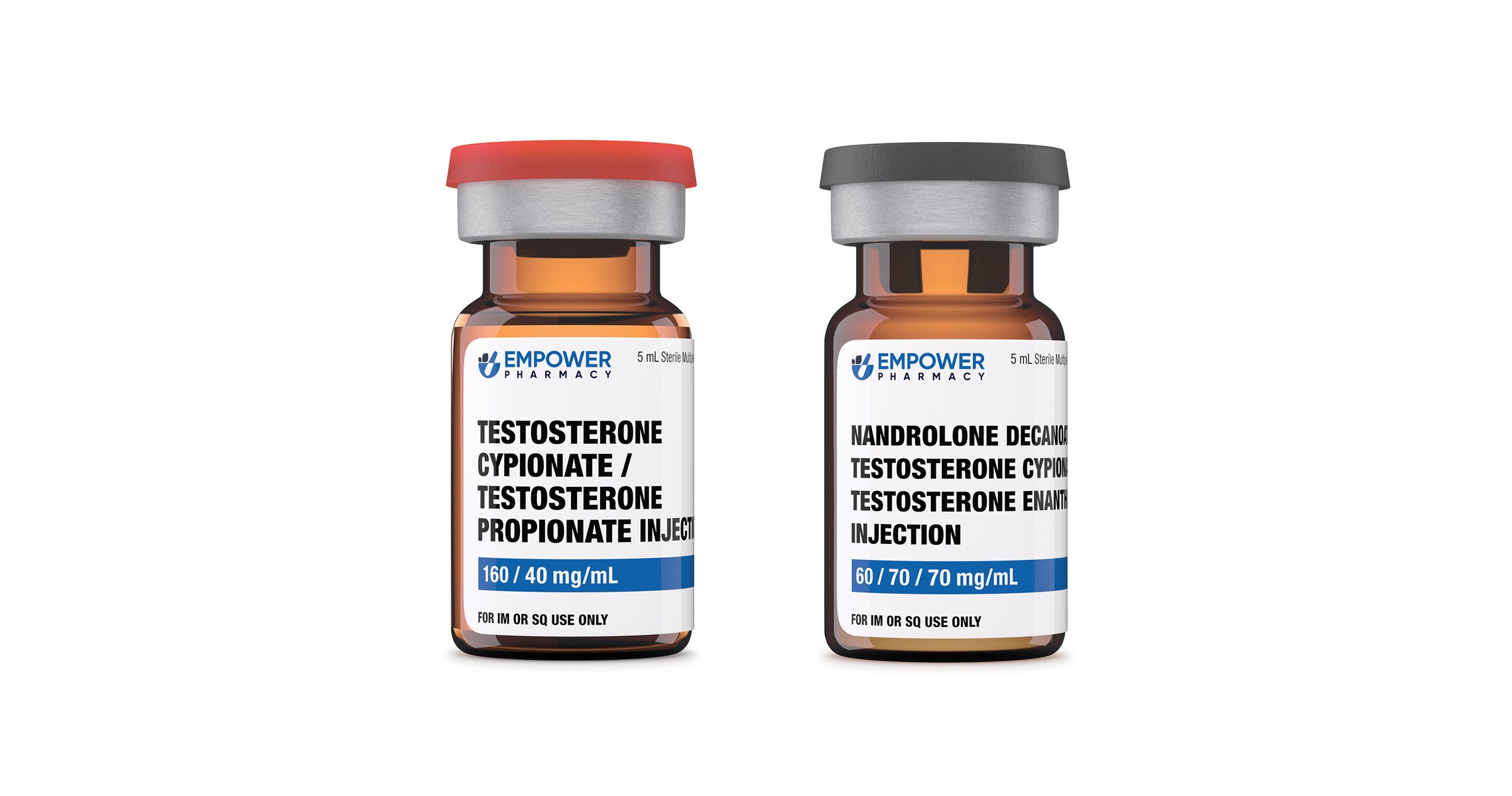
Testosterone cypionate and enanthate don't carry the same POME risk profile, so they don't require REMS programs. Patients can self-inject at home.
The practical impact:
This is a significant barrier to Aveed adoption in the US despite its convenient dosing schedule (every 10 weeks after loading). Many physicians find the registration and monitoring requirements burdensome, and patients dislike mandatory office visits for every injection. It's one reason Aveed hasn't captured more market share despite offering a genuinely useful longer-acting option.
Outside the US, Nebido faces fewer restrictions in most countries, though administration protocols vary by region.
 www.empowerpharmacy.com
www.empowerpharmacy.com