Nelson Vergel
Founder, ExcelMale.com
Serum Sex Hormone-Binding Globulin and Testosterone In Relation To Cardiovascular Disease Risk Factors
Canoy D, Barber TM, Pouta A, et al. European Journal of Endocrinology. http://www.eje-online.org/content/early/2014/03/26/EJE-13-1046.abstract
Objective: Reduced sex hormone-binding globulin (SHBG) concentration predicts insulin resistance and type 2 diabetes but its association with cardiovascular disease (CVD) risk is unclear. We examined the association between SHBG and cardiovascular risk factors, independently of total testosterone (TT), in young men.
Design: Observational, cross-sectional study
Setting: General community
Participants: 2,716 31-year old men in the 1966 Northern Finland Birth Cohort with clinical examination data and fasting blood samples.
Outcome variables: Blood pressure (BP), lipids and C-reactive protein (CRP) as biological CVD risk markers.
Results: SHBG concentration was significantly and inversely related to systolic and diastolic BP, triglycerides and CRP but positively to high-density lipoprotein (HDL) cholesterol after adjusting for insulin, body mass index, waist circumference, smoking, education and physical activity (all P <0.05). These linearly graded associations persisted with additional adjustment for TT. SHBG was significantly associated with total cholesterol only with adjustment for covariates and TT (P <0.05).
The direction and magnitude of associations between TT and risk factors were variable but further adjustment for insulin, adiposity and SHBG showed positive associations between TT and blood pressure, total and low-density lipoprotein cholesterol and triglycerides and an inverse association with CRP (all P<0.05), but its relation with HDL-cholesterol was no longer significant.
Conclusions: In this cohort of young adult men, higher SHBG concentration was associated with a more favourable CVD risk profile, independently of TT. SHBG concentration modified the associations of TT with CVD risk factors.
****
Note:
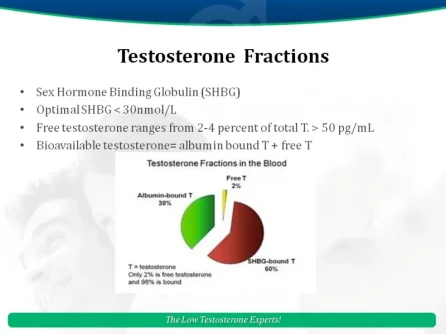
In a healthy young male, about 60 percent of his testosterone is attached to sex hormone binding globulin (SHBG). Hormones bound to SHBG can't be used by the body and lose their anabolic effect. SHBG is produced mostly by the liver and is released into the bloodstream.SHBG has both enhancing and inhibiting hormonal influences. It decreases with high levels of insulin, growth hormone, insulin-like growth factor 1 (IGF-1), androgens, prolactin and transcortin. High estrogen, and thyroxine cause it to increase.
SHBG levels are decreased by administration of testosterone and anabolic steroids,polycystic ovary syndrome, hypothyroidism, diabetes, obesity, Cushing's syndrome, and acromegaly. SHBG levels increase with estrogenic states (oral contraceptives), pregnancy, hyperthyroidism, cirrhosis, anorexia nervosa, and certain drugs. Long-term calorie restriction of more than 50 percent increases SHBG, while lowering free and total testosterone and estradiol.
Some studies show that low protein diets may increase SHBG which suggests that in elderly men a high protein diet could increase bioavailable testosterone and mitigate the effects of the age-related decrease in that hormone. Intervention studies will be necessary to verify this.
Canoy D, Barber TM, Pouta A, et al. European Journal of Endocrinology. http://www.eje-online.org/content/early/2014/03/26/EJE-13-1046.abstract
Objective: Reduced sex hormone-binding globulin (SHBG) concentration predicts insulin resistance and type 2 diabetes but its association with cardiovascular disease (CVD) risk is unclear. We examined the association between SHBG and cardiovascular risk factors, independently of total testosterone (TT), in young men.
Design: Observational, cross-sectional study
Setting: General community
Participants: 2,716 31-year old men in the 1966 Northern Finland Birth Cohort with clinical examination data and fasting blood samples.
Outcome variables: Blood pressure (BP), lipids and C-reactive protein (CRP) as biological CVD risk markers.
Results: SHBG concentration was significantly and inversely related to systolic and diastolic BP, triglycerides and CRP but positively to high-density lipoprotein (HDL) cholesterol after adjusting for insulin, body mass index, waist circumference, smoking, education and physical activity (all P <0.05). These linearly graded associations persisted with additional adjustment for TT. SHBG was significantly associated with total cholesterol only with adjustment for covariates and TT (P <0.05).
The direction and magnitude of associations between TT and risk factors were variable but further adjustment for insulin, adiposity and SHBG showed positive associations between TT and blood pressure, total and low-density lipoprotein cholesterol and triglycerides and an inverse association with CRP (all P<0.05), but its relation with HDL-cholesterol was no longer significant.
Conclusions: In this cohort of young adult men, higher SHBG concentration was associated with a more favourable CVD risk profile, independently of TT. SHBG concentration modified the associations of TT with CVD risk factors.
****
Note:
In a healthy young male, about 60 percent of his testosterone is attached to sex hormone binding globulin (SHBG). Hormones bound to SHBG can't be used by the body and lose their anabolic effect. SHBG is produced mostly by the liver and is released into the bloodstream.SHBG has both enhancing and inhibiting hormonal influences. It decreases with high levels of insulin, growth hormone, insulin-like growth factor 1 (IGF-1), androgens, prolactin and transcortin. High estrogen, and thyroxine cause it to increase.
SHBG levels are decreased by administration of testosterone and anabolic steroids,polycystic ovary syndrome, hypothyroidism, diabetes, obesity, Cushing's syndrome, and acromegaly. SHBG levels increase with estrogenic states (oral contraceptives), pregnancy, hyperthyroidism, cirrhosis, anorexia nervosa, and certain drugs. Long-term calorie restriction of more than 50 percent increases SHBG, while lowering free and total testosterone and estradiol.
Some studies show that low protein diets may increase SHBG which suggests that in elderly men a high protein diet could increase bioavailable testosterone and mitigate the effects of the age-related decrease in that hormone. Intervention studies will be necessary to verify this.
Attachments
Last edited: