madman
Super Moderator
The role of gonadotropins in testicular and adrenal androgen biosynthesis pathways -insights from males with congenital hypogonadotropic hypogonadism on hCG/rFSH and on testosterone replacement
SUMMARY
Objective: To delineate the role of gonadotropins in male androgen biosynthesis pathways
Design: Case-control study
Patients and measurements: 25 males with congenital hypogonadotropic hypogonadism (CHH) underwent hCG/rFSH and testosterone treatment sequentially. Serum steroid hormone profiles (testosterone precursors and metabolites) on both replacement regimens were analyzed, using liquid chromatography-tandem mass spectrometry (LC-MS/MS) and compared to those of healthy controls, matched by age, BMI, and serum testosterone.
Results: On testosterone replacement, serum concentrations of the classic Δ4 pathway hormones progesterone and 17-hydroxy-progesterone (17-OHP), and the marker steroid of an alternative pathway of testosterone synthesis (androstenediol) were decreased, compared to controls. Androstanediol, a marker of the backdoor pathway of dihydrotestosterone (DHT) synthesis, was increased. 17-OH-pregnenolone, androstenedione, and DHEAS (Δ5 pathway), three 11-oxygenated C19 androgens (11-keto-A4, 11-keto-T, and 11-keto-DHT), and the testosterone (T) metabolites DHT and 17ß-estradiol (E2) were similar to controls.
On gonadotropin replacement, 17-OHP, 17-OH-pregnenolone, DHEAS and androstenedione, as well as DHT, androstenediol, and all 11-oxygenated C19 androgens were normal. Progesterone (Δ4 pathway) was slightly decreased, androstanediol (backdoor DHT pathway) and E2 (T metabolite) were increased.
Conclusions: In males with CHH, serum steroid hormone profiles resemble those of healthy men, if hCG/rFSH is used for substitution. Gonadotropins contribute to steroid hormone production along the classic Δ4 pathway and co-activate an alternative pathway of testosterone biosynthesis via androstenediol. Backdoor DHT biosynthesis, Δ5 17-OH-pregnenolone, DHEA(S), and androstenedione synthesis and 11- oxygenated C19 androgen production are activated independently of gonadotropins. The androgen replacement modality used for the treatment of hypogonadal males with absent or reduced endogenous LH/FSH- secretion may impact long term health and quality of life.
Introduction
Androgens are a family of steroid hormones important for male sexual development, for reproductive health, and metabolic homeostasis. The “classic” androgens, testosterone (T) and dihydrotestosterone (DHT) are C19 carbon steroid hormones, synthesized in the testes from cholesterol via different steroidogenic pathways. Androgens are also produced in the adrenal zona reticularis or locally, in target tissues, by conversion from circulating C21 androgen precursor steroids 1. Steroidogenic enzymes, involved in the formation of T and DHT and differentially expressed and activated in gonadal and adrenal tissues include 3ß-hydroxysteroid-dehydrogenase (HSD3B2), 17α-hydroxylase/C17-20-lyase (CYP17A1), 17ß-hydroxysteroid-dehydrogenase (HSD17B3 and 5), and 5α-reductase (SRD5A2) (Figure1). While androgen production in Leydig cells is dependent on stimulation by luteinizing hormone (LH), produced by gonadotropic anterior pituitary cells, adrenal steroid secretion is regulated by adrenocorticotropic hormone (ACTH) from corticotropic pituitary cells.
The biological effects mediated by androgens are conveyed through the androgen receptor (AR; NR3C4), a ligand-activated nuclear receptor that functions as a transcription factor, and regulates gene expression in target tissues, and that is present in reproductive organs, brain, bone, heart, liver, skin, and larynx 2. Differential androgenic effects are conveyed by the relative concentrations of the respective androgenic steroids in circulation and are further modulated by other factors (their binding to SHBG or albumin in serum with consequences on clearing rates 3, the passive influx of active transport into target cells, specific affinities to the AR, distinct promotor activation profiles 4. Further regulation of AR activity is conveyed by variation in length of a glutamine repeat region (encoded by a polymorphic (CAG)n repeat in exon 1) present at the NH2-terminal domain of the AR 5.
In the human male, the virilizing properties of T and DHT cause internal and external sexual differentiation during fetal life, resulting in the “male primary sexual characteristics” 6. The pubertal increase of circulating testosterone and its maintenance at adult male concentrations in serum is responsible for both virilizing and anabolic effects, resulting in male secondary sexual characteristics, muscle accrual, bone mineralization, and stimulation of erythropoiesis.
Beyond T and DHT, precursor steroids and metabolites are able to elicit androgenic action. The role of these androgenic steroids has been established in conditions accompanied by androgen excess, such as congenital adrenal hyperplasia 7, polycystic ovary syndrome 8, and castration-resistant prostate cancer 9; however, their contribution to androgenic action in the healthy male is as yet unclear. The impact of gonadotropins on the secretion of bioactive androgenic steroids and their precursors is equally unresolved. Males with congenital hypogonadotropic hypogonadism (CHH) display central hormone deficiency, with disturbed secretion or action of hypothalamic GnRH on the anterior pituitary gland. As a consequence, LH and FSH stimulation of the gonads is deficient. CHH can thus be viewed as a naturally occurring human “knockdown” of gonadotropin stimulation of the gonads, with uncompromised ACTH secretion. To delineate the role of gonadotropins in testicular and adrenal androgen biosynthesis pathways, we analyzed steroid hormone profiles in serum of CHH males twice, once, while patients were on testosterone and once, while they were on gonadotropin replacement.
Results
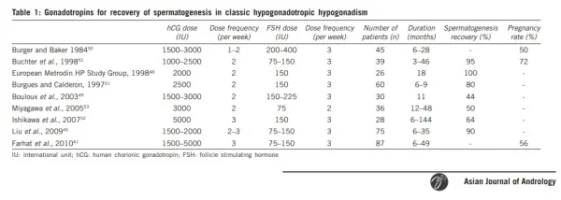
Combined treatment of CHH males with hCG and rFSH resulted in steroid hormone profiles similar to those of healthy men, but this was not the case, while exogenous testosterone was used for replacement. Serum steroid hormone levels on the different treatment modalities in CHH males and matched controls are summarized in Table 1 and plotted individually in Figure 3 and Figure 4. While CHH patients were on T substitution, decreased serum concentrations of some members of the classical Δ4 pathway of androgen biosynthesis (progesterone (p=0.0104), 17-OH-progesterone (17 OHP) (p<0.0001)) and of the alternative T pathway steroid androstenediol (p=0.004)) were observed, compared to controls. The marker steroid of the backdoor DHT pathway androstandiol (p=0.025), was slightly increased.
The testosterone metabolites DHT and 17-ß estradiol (E2), the Δ5 steroid 17-pregnenolone, the sulfated form of the Δ5 pathway steroid dehydroepiandrosterone DHEA, i.e. dehydroepiandrosterone sulfate (DHEAS), androstenedione (A4) and all measured 11-oxygenated C19 androgens (11-keto-testosterone (11-K-T), 11-keto-dihydro-testosterone (11-K-DHT) and 11-keto-androstenedione (11-K-A4)) were comparable to those of controls.
By contrast, normal concentrations were found for most steroid hormones in the serum of CHH males, while they were on hCG/rFSH replacement. Specifically, steroid profiles resembled those of healthy male controls, regarding the Δ 4 pathway of androgen biosynthesis (17-OHP) and the metabolite DHT, the marker steroid of an alternative T pathway via androstenediol, the Δ5 pathway steroids Δ5 steroid 17- pregnenolone, DHEAS and A4 and all aforementioned 11-oxygenated C19 androgens (11-K-A4, 11-K-T, 11-K-DHT). Serum progesterone was slightly decreased (p=0.0104), the testosterone metabolite E2 and the backdoor DHT pathway steroid androstanediol were increased (both p<0.0001).
Discussion
An optimal endocrine replacement strategy for hypogonadotropic hypogonadal males aims at normalizing all aspects of deficient androgenic action. While testosterone replacement has been used in clinical practice to solely convey androgenic effects, gonadotropins have been employed for the purpose of additionally initiating testicular growth and spermatogenesis 13.
The present study provides data on steroid hormone profiles of males with CHH, in which these two different replacement regimens were applied sequentially. The hormone concentrations in serum reflect the overall production of the hormone that is contributed to the bloodstream by each hormone-producing tissue. The naturally occurring “knockdown condition” of central hormonal stimulation of gonads, with uncompromised ACTH secretion that is present in CHH males, was used as a model, to enable delineation of gonadotropin effects on testicular and adrenal steroidogenic pathways involved in male androgen biosynthesis. Specifically, hCG/rFSH-effects on serum steroid hormone concentrations of the classic Δ5 pathway of steroid biosynthesis, on concentrations of steroids of the Δ4 steroidogenic pathway, the alternative pathway of testosterone biosynthesis, the backdoor pathway of DHT synthesis, and on concentrations of the 11-oxygenated C19 androgen pathway were investigated. In addition, the serum levels of testosterone metabolites were investigated.
Our results indicate that the treatment of CHH males with gonadotropins results in steroid hormone profiles similar to those of healthy men, with few exceptions (E2, progesterone). However, this is not the case using a regimen based on exogenous testosterone. If testosterone is applied, steroidogenic pathways in testicles of CHH males remain unstimulated. By contrast, if hCG +rFSH are used, the LHCG receptor in Leydig cells is activated 14. In response, multiple steroids of the classical steroidogenic cascade are synthesized by the gonads, including the classic potent androgens T and DHT. This explains the differences observed in serum steroid levels in CHH males on the two different replacement regimens.
Summarized results and conclusions
These biochemical studies of serum steroid hormone patterns in CHH males on two different androgenic replacement regimens contribute to our knowledge of human steroidogenesis, specifically androgen production and it's regulation. Gonadotropins contribute to steroid production along the classic Δ4 pathway, by stimulation of 17-OHP production. In addition, gonadotropins co-activate an alternative pathway of T biosynthesis from DHEA via androstenediol.
However, Δ5 biosynthesis of 17-OH-pregnenolone, DHEA(S) seems fully gonadotropin-independent, and the production of androstenedione is largely gonadotropin-independent. Thus, an “adrenal-peripheral tissues-testicular collaboration” regarding androgen synthesis by classic or alternative pathways seems possible.
The 11-oxygenated C19 androgen pathway is activated independently of gonadotropins. The activity of the three DHT backdoor pathways (converging in androstanediol biosynthesis) is not increased by gonadotropins.
A replacement regimen with combined hCG/rFSH mimics physiologic steroid hormone profiles better than a substitution with exogenous testosterone. The documented differences in steroid profiles on testosterone replacement in hypogonadal males with absent or severely reduced endogenous LH and FSH secretion may have long term consequences for health and wellbeing. Specifically, body composition, bone health, glucose, and lipid metabolism, salt and water balance, cognition, mood, sleep, and sexual function could be affected. The steroidogenic differences could also be relevant for gonadotropin-suppressive treatments with long-acting testosterone preparations in males with primary hypogonadism. To what extent this hypothesis is true, should be addressed in future clinical studies.
SUMMARY
Objective: To delineate the role of gonadotropins in male androgen biosynthesis pathways
Design: Case-control study
Patients and measurements: 25 males with congenital hypogonadotropic hypogonadism (CHH) underwent hCG/rFSH and testosterone treatment sequentially. Serum steroid hormone profiles (testosterone precursors and metabolites) on both replacement regimens were analyzed, using liquid chromatography-tandem mass spectrometry (LC-MS/MS) and compared to those of healthy controls, matched by age, BMI, and serum testosterone.
Results: On testosterone replacement, serum concentrations of the classic Δ4 pathway hormones progesterone and 17-hydroxy-progesterone (17-OHP), and the marker steroid of an alternative pathway of testosterone synthesis (androstenediol) were decreased, compared to controls. Androstanediol, a marker of the backdoor pathway of dihydrotestosterone (DHT) synthesis, was increased. 17-OH-pregnenolone, androstenedione, and DHEAS (Δ5 pathway), three 11-oxygenated C19 androgens (11-keto-A4, 11-keto-T, and 11-keto-DHT), and the testosterone (T) metabolites DHT and 17ß-estradiol (E2) were similar to controls.
On gonadotropin replacement, 17-OHP, 17-OH-pregnenolone, DHEAS and androstenedione, as well as DHT, androstenediol, and all 11-oxygenated C19 androgens were normal. Progesterone (Δ4 pathway) was slightly decreased, androstanediol (backdoor DHT pathway) and E2 (T metabolite) were increased.
Conclusions: In males with CHH, serum steroid hormone profiles resemble those of healthy men, if hCG/rFSH is used for substitution. Gonadotropins contribute to steroid hormone production along the classic Δ4 pathway and co-activate an alternative pathway of testosterone biosynthesis via androstenediol. Backdoor DHT biosynthesis, Δ5 17-OH-pregnenolone, DHEA(S), and androstenedione synthesis and 11- oxygenated C19 androgen production are activated independently of gonadotropins. The androgen replacement modality used for the treatment of hypogonadal males with absent or reduced endogenous LH/FSH- secretion may impact long term health and quality of life.
Introduction
Androgens are a family of steroid hormones important for male sexual development, for reproductive health, and metabolic homeostasis. The “classic” androgens, testosterone (T) and dihydrotestosterone (DHT) are C19 carbon steroid hormones, synthesized in the testes from cholesterol via different steroidogenic pathways. Androgens are also produced in the adrenal zona reticularis or locally, in target tissues, by conversion from circulating C21 androgen precursor steroids 1. Steroidogenic enzymes, involved in the formation of T and DHT and differentially expressed and activated in gonadal and adrenal tissues include 3ß-hydroxysteroid-dehydrogenase (HSD3B2), 17α-hydroxylase/C17-20-lyase (CYP17A1), 17ß-hydroxysteroid-dehydrogenase (HSD17B3 and 5), and 5α-reductase (SRD5A2) (Figure1). While androgen production in Leydig cells is dependent on stimulation by luteinizing hormone (LH), produced by gonadotropic anterior pituitary cells, adrenal steroid secretion is regulated by adrenocorticotropic hormone (ACTH) from corticotropic pituitary cells.
The biological effects mediated by androgens are conveyed through the androgen receptor (AR; NR3C4), a ligand-activated nuclear receptor that functions as a transcription factor, and regulates gene expression in target tissues, and that is present in reproductive organs, brain, bone, heart, liver, skin, and larynx 2. Differential androgenic effects are conveyed by the relative concentrations of the respective androgenic steroids in circulation and are further modulated by other factors (their binding to SHBG or albumin in serum with consequences on clearing rates 3, the passive influx of active transport into target cells, specific affinities to the AR, distinct promotor activation profiles 4. Further regulation of AR activity is conveyed by variation in length of a glutamine repeat region (encoded by a polymorphic (CAG)n repeat in exon 1) present at the NH2-terminal domain of the AR 5.
In the human male, the virilizing properties of T and DHT cause internal and external sexual differentiation during fetal life, resulting in the “male primary sexual characteristics” 6. The pubertal increase of circulating testosterone and its maintenance at adult male concentrations in serum is responsible for both virilizing and anabolic effects, resulting in male secondary sexual characteristics, muscle accrual, bone mineralization, and stimulation of erythropoiesis.
Beyond T and DHT, precursor steroids and metabolites are able to elicit androgenic action. The role of these androgenic steroids has been established in conditions accompanied by androgen excess, such as congenital adrenal hyperplasia 7, polycystic ovary syndrome 8, and castration-resistant prostate cancer 9; however, their contribution to androgenic action in the healthy male is as yet unclear. The impact of gonadotropins on the secretion of bioactive androgenic steroids and their precursors is equally unresolved. Males with congenital hypogonadotropic hypogonadism (CHH) display central hormone deficiency, with disturbed secretion or action of hypothalamic GnRH on the anterior pituitary gland. As a consequence, LH and FSH stimulation of the gonads is deficient. CHH can thus be viewed as a naturally occurring human “knockdown” of gonadotropin stimulation of the gonads, with uncompromised ACTH secretion. To delineate the role of gonadotropins in testicular and adrenal androgen biosynthesis pathways, we analyzed steroid hormone profiles in serum of CHH males twice, once, while patients were on testosterone and once, while they were on gonadotropin replacement.
Results
Combined treatment of CHH males with hCG and rFSH resulted in steroid hormone profiles similar to those of healthy men, but this was not the case, while exogenous testosterone was used for replacement. Serum steroid hormone levels on the different treatment modalities in CHH males and matched controls are summarized in Table 1 and plotted individually in Figure 3 and Figure 4. While CHH patients were on T substitution, decreased serum concentrations of some members of the classical Δ4 pathway of androgen biosynthesis (progesterone (p=0.0104), 17-OH-progesterone (17 OHP) (p<0.0001)) and of the alternative T pathway steroid androstenediol (p=0.004)) were observed, compared to controls. The marker steroid of the backdoor DHT pathway androstandiol (p=0.025), was slightly increased.
The testosterone metabolites DHT and 17-ß estradiol (E2), the Δ5 steroid 17-pregnenolone, the sulfated form of the Δ5 pathway steroid dehydroepiandrosterone DHEA, i.e. dehydroepiandrosterone sulfate (DHEAS), androstenedione (A4) and all measured 11-oxygenated C19 androgens (11-keto-testosterone (11-K-T), 11-keto-dihydro-testosterone (11-K-DHT) and 11-keto-androstenedione (11-K-A4)) were comparable to those of controls.
By contrast, normal concentrations were found for most steroid hormones in the serum of CHH males, while they were on hCG/rFSH replacement. Specifically, steroid profiles resembled those of healthy male controls, regarding the Δ 4 pathway of androgen biosynthesis (17-OHP) and the metabolite DHT, the marker steroid of an alternative T pathway via androstenediol, the Δ5 pathway steroids Δ5 steroid 17- pregnenolone, DHEAS and A4 and all aforementioned 11-oxygenated C19 androgens (11-K-A4, 11-K-T, 11-K-DHT). Serum progesterone was slightly decreased (p=0.0104), the testosterone metabolite E2 and the backdoor DHT pathway steroid androstanediol were increased (both p<0.0001).
Discussion
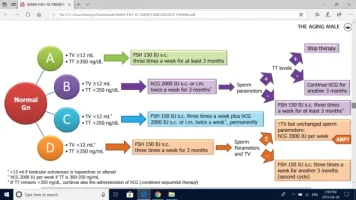
An optimal endocrine replacement strategy for hypogonadotropic hypogonadal males aims at normalizing all aspects of deficient androgenic action. While testosterone replacement has been used in clinical practice to solely convey androgenic effects, gonadotropins have been employed for the purpose of additionally initiating testicular growth and spermatogenesis 13.
The present study provides data on steroid hormone profiles of males with CHH, in which these two different replacement regimens were applied sequentially. The hormone concentrations in serum reflect the overall production of the hormone that is contributed to the bloodstream by each hormone-producing tissue. The naturally occurring “knockdown condition” of central hormonal stimulation of gonads, with uncompromised ACTH secretion that is present in CHH males, was used as a model, to enable delineation of gonadotropin effects on testicular and adrenal steroidogenic pathways involved in male androgen biosynthesis. Specifically, hCG/rFSH-effects on serum steroid hormone concentrations of the classic Δ5 pathway of steroid biosynthesis, on concentrations of steroids of the Δ4 steroidogenic pathway, the alternative pathway of testosterone biosynthesis, the backdoor pathway of DHT synthesis, and on concentrations of the 11-oxygenated C19 androgen pathway were investigated. In addition, the serum levels of testosterone metabolites were investigated.
Our results indicate that the treatment of CHH males with gonadotropins results in steroid hormone profiles similar to those of healthy men, with few exceptions (E2, progesterone). However, this is not the case using a regimen based on exogenous testosterone. If testosterone is applied, steroidogenic pathways in testicles of CHH males remain unstimulated. By contrast, if hCG +rFSH are used, the LHCG receptor in Leydig cells is activated 14. In response, multiple steroids of the classical steroidogenic cascade are synthesized by the gonads, including the classic potent androgens T and DHT. This explains the differences observed in serum steroid levels in CHH males on the two different replacement regimens.
Summarized results and conclusions
These biochemical studies of serum steroid hormone patterns in CHH males on two different androgenic replacement regimens contribute to our knowledge of human steroidogenesis, specifically androgen production and it's regulation. Gonadotropins contribute to steroid production along the classic Δ4 pathway, by stimulation of 17-OHP production. In addition, gonadotropins co-activate an alternative pathway of T biosynthesis from DHEA via androstenediol.
However, Δ5 biosynthesis of 17-OH-pregnenolone, DHEA(S) seems fully gonadotropin-independent, and the production of androstenedione is largely gonadotropin-independent. Thus, an “adrenal-peripheral tissues-testicular collaboration” regarding androgen synthesis by classic or alternative pathways seems possible.
The 11-oxygenated C19 androgen pathway is activated independently of gonadotropins. The activity of the three DHT backdoor pathways (converging in androstanediol biosynthesis) is not increased by gonadotropins.
A replacement regimen with combined hCG/rFSH mimics physiologic steroid hormone profiles better than a substitution with exogenous testosterone. The documented differences in steroid profiles on testosterone replacement in hypogonadal males with absent or severely reduced endogenous LH and FSH secretion may have long term consequences for health and wellbeing. Specifically, body composition, bone health, glucose, and lipid metabolism, salt and water balance, cognition, mood, sleep, and sexual function could be affected. The steroidogenic differences could also be relevant for gonadotropin-suppressive treatments with long-acting testosterone preparations in males with primary hypogonadism. To what extent this hypothesis is true, should be addressed in future clinical studies.
Attachments
Last edited by a moderator: