TL;DR: Some research suggests that echinacoside may complement a SERM in reducing TRT-induced negative HPT-axis feedback at the hypothalamus.
Background: In testosterone replacement therapy, elevated levels of testosterone and estradiol apply negative feedback to the hypothalamus. This suppresses the release of kisspeptin, which in turn suppresses the production of gonadotropin releasing hormone (GnRH). The lack of GnRH in turn suppresses production of LH and FSH at the pituitary,† which can then lead to a loss of endogenous testosterone production, testicular atrophy and infertility. It's hypothesized that some men experience other side effects caused directly by the reduction in upstream hormones.
Various treatments have been used to counteract HPTA suppression under TRT:
• HCG Human Chorionic Gonadotropin (hCG) is the best known. HCG acts as a replacement for LH. It stimulates the Leydig cells, which can lessen testicular atrophy and restore fertility in many cases. Subjective benefits are often reported. HCG does not help with the loss of FSH and the upstream hormones.
• SERMs Because selective estrogen receptor modulators (SERMs) are known to stimulate the HPTA in normal men and women, they have been used with TRT in an attempt to keep the HPTA going. However, this appears to fail most of the time. The reason why is that SERMs are limited to blocking negative feedback from estradiol at the hypothalamus and pituitary. The negative feedback of testosterone at the hypothalamus is left unchecked.
• High-dose GnRH Royal Medical Center has published numerous case studies suggesting that once- or twice-weekly high doses of GnRH can stimulate production of LH and FSH. It may be that the relatively high doses overcome estradiol's negative feedback at the pituitary. Our assumption is that each isolated injection results in only single pulses of LH and FSH, a far cry from endogenous patterns. It's unclear if this is sufficient to do things like reverse testicular atrophy or restore fertility.
• Low-dose GnRH Described here, this complicated treatment bypasses the hypothalamus, using pulsed physiological doses of GnRH to stimulate the pituitary to produce LH and FSH. A SERM is used to prevent negative feedback from estradiol at the pituitary.
Discussion: In commenting over the years on the failure of TRT + SERM to maintain HPTA function, I have noted that we need a selective androgen receptor modular (SARM) to add to this to make it work; the ideal SARM would block negative feedback from androgens at the hypothalamus. Now, thanks to a tip from @ajax31, I see that there is a potential candidate that has been hiding in plain sight:
 www.nature.com
www.nature.com
Those in-the-know may already have recalled that echinacoside is a significant component of plants in the Cistanche genus. In the U.S., Cistanche plant extracts are readily available as dietary supplements. Cistanche is mentioned a few times in the forum, sometimes in the context of post-cycle treatment. This supplement has definitely been on the radar as an HPTA stimulator. It's just not obvious to me if it has been used in conjunction with TRT.
Conclusion: There is a chance that adding enclomiphene and Cistanche plant extract to a TRT protocol would result in HTPA activity. Even if this works, there is uncertainty about the subjective results. Anecdotally, we have seen several men experiencing poor subjective results with enclomiphene monotherapy, in spite of good numbers. Would the same apply to this combo therapy, or does the exogenous testosterone create a different situation? Speaking for myself, I continue to have good results with a protocol that includes both exogenous testosterone and enclomiphene. I could be an outlier, but only time and experimentation will tell.
†Estradiol also applies negative feedback directly to the pituitary.
Background: In testosterone replacement therapy, elevated levels of testosterone and estradiol apply negative feedback to the hypothalamus. This suppresses the release of kisspeptin, which in turn suppresses the production of gonadotropin releasing hormone (GnRH). The lack of GnRH in turn suppresses production of LH and FSH at the pituitary,† which can then lead to a loss of endogenous testosterone production, testicular atrophy and infertility. It's hypothesized that some men experience other side effects caused directly by the reduction in upstream hormones.
Various treatments have been used to counteract HPTA suppression under TRT:
• HCG Human Chorionic Gonadotropin (hCG) is the best known. HCG acts as a replacement for LH. It stimulates the Leydig cells, which can lessen testicular atrophy and restore fertility in many cases. Subjective benefits are often reported. HCG does not help with the loss of FSH and the upstream hormones.
• SERMs Because selective estrogen receptor modulators (SERMs) are known to stimulate the HPTA in normal men and women, they have been used with TRT in an attempt to keep the HPTA going. However, this appears to fail most of the time. The reason why is that SERMs are limited to blocking negative feedback from estradiol at the hypothalamus and pituitary. The negative feedback of testosterone at the hypothalamus is left unchecked.
• High-dose GnRH Royal Medical Center has published numerous case studies suggesting that once- or twice-weekly high doses of GnRH can stimulate production of LH and FSH. It may be that the relatively high doses overcome estradiol's negative feedback at the pituitary. Our assumption is that each isolated injection results in only single pulses of LH and FSH, a far cry from endogenous patterns. It's unclear if this is sufficient to do things like reverse testicular atrophy or restore fertility.
• Low-dose GnRH Described here, this complicated treatment bypasses the hypothalamus, using pulsed physiological doses of GnRH to stimulate the pituitary to produce LH and FSH. A SERM is used to prevent negative feedback from estradiol at the pituitary.
Discussion: In commenting over the years on the failure of TRT + SERM to maintain HPTA function, I have noted that we need a selective androgen receptor modular (SARM) to add to this to make it work; the ideal SARM would block negative feedback from androgens at the hypothalamus. Now, thanks to a tip from @ajax31, I see that there is a potential candidate that has been hiding in plain sight:
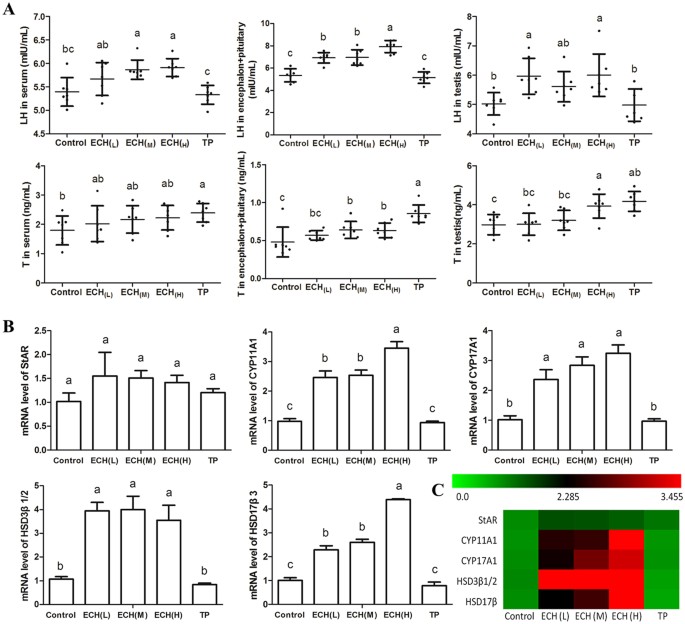
... these data demonstrate that [echinacoside] blocks [androgen receptor] activity in the hypothalamus to increase the quantity of sperm and protect against oligoasthenospermia in rats.
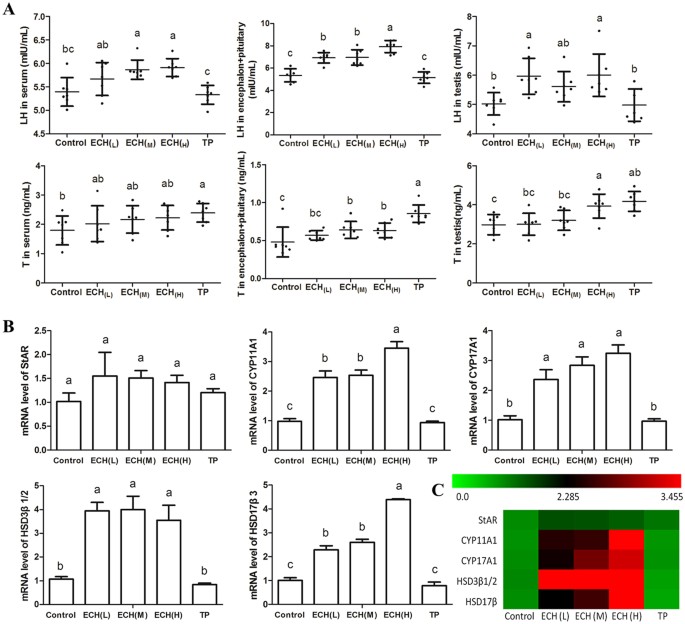
Echinacoside Increases Sperm Quantity in Rats by Targeting the Hypothalamic Androgen Receptor - Scientific Reports
Male infertility is a major health issue with an estimated prevalence of 4.2% of male infertility worldwide. Our early work demonstrated that Cistanche extracts protect against sperm damage in mice and that echinacoside (ECH) is one of the major active components. Here we report an essential...
Those in-the-know may already have recalled that echinacoside is a significant component of plants in the Cistanche genus. In the U.S., Cistanche plant extracts are readily available as dietary supplements. Cistanche is mentioned a few times in the forum, sometimes in the context of post-cycle treatment. This supplement has definitely been on the radar as an HPTA stimulator. It's just not obvious to me if it has been used in conjunction with TRT.
Conclusion: There is a chance that adding enclomiphene and Cistanche plant extract to a TRT protocol would result in HTPA activity. Even if this works, there is uncertainty about the subjective results. Anecdotally, we have seen several men experiencing poor subjective results with enclomiphene monotherapy, in spite of good numbers. Would the same apply to this combo therapy, or does the exogenous testosterone create a different situation? Speaking for myself, I continue to have good results with a protocol that includes both exogenous testosterone and enclomiphene. I could be an outlier, but only time and experimentation will tell.
†Estradiol also applies negative feedback directly to the pituitary.















