Note:HCG mimics LH but it is not LH and it's not picked up by the LH blood test. In fact, it suppresses LH like endogeneous testosterone does. But the amazing thing that the study below found is that HCG can increase sperm production and quality even in the absence of LH AND FSH. Most researchers believed that without FSH there was no possible sperm production.
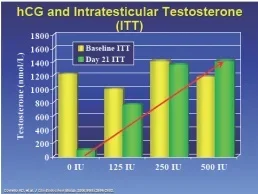
The second study shows that testosterone inside the testicles (instratesticular testosterone or ITT) has to reach a certain amount for Sertoli cells to "wake up" to produce sperm. TRT actually decreases testosterone inside the cells by an unknown mechanism. HCG doses under 300 IU along with TRT may not normalize intratesticular testosterone since 250 IU produced an ITT 7% below baseline. 500 IU produced ITT 25% above normal. The Baylor study below used the 500 IU dose.
Conclusion: Do not use anything below 500 IU if you want to normalize your ITT while on TRT. No studies have been done on twice per week injection frequency, but that dose may work to prevent testicular atrophy (anecdotally). Three times per week or more may be needed to preserve fertility while on TRT. However, 33% of men (mostly older and who have been on TRT the longest prior to introducing hCG) do not respond as well to TRT+hCG when it comes to sperm quantity and quality. Those men may be better off on hCG+FSH.
Testosterone+ HCG Preserves Healthy Sperm in Men on Testosterone Replacement Therapy (Injections and gels)
Tung-Chin Hsieh, Alexander W. Pastuszak, Kathleen Hwang and Larry I. Lipshultz*,†
From the Division of Urology, University of California-San Diego (TCH), San Diego, California, Scott Department of Urology, Baylor College of Medicine (AWP, LIL), Houston, Texas, and Department of Urology (KH), Brown University School of Medicine, Providence, Rhode Island
Purpose: Testosterone replacement therapy results in decreased serum gonadotropins (hormones produced by the pituitary gland- LH and FSH- that jump start testicular function) and intratesticular testosterone (inside the testicles), and impairs spermatogenesis (sperm production), leading to azoospermia (no viable sperm) in 40% of patients. However, intratesticular testosterone can be maintained during testosterone replacement therapy with co-administration of low dose human chorionic gonadotropin, which may support continued spermatogenesis in patients on testosterone replacement therapy.
Materials and Methods: We retrospectively reviewed the records of hypogonadal men treated with testosterone replacement therapy and concomitant low dose human chorionic gonadotropin(HCG). Testosterone replacement consisted of daily topical gel or weekly intramuscular injection with intramuscular human chorionic gonadotropin (500 IU) every other day. Serum and free testosterone,estradiol, semen parameters and pregnancy rates were evaluated before and during therapy.
Results: A total of 26 men with a mean age of 35.9 years were included in the study. Mean followup was 6.2 months. Of the men 19 were treated with injectable testosterone and 7 were treated with transdermal gel. Mean serum hormone levels before vs during treatment were testosterone 207.2 vs 1,055.5 ng/dl (p<0.0001), free testosterone 8.1 vs 20.4 pg/ml (p = 0.02) and estradiol 2.2 vs 3.7 pg/ml (p = 0.11). Pretreatment semen parameters were volume 2.9 ml, density 35.2 million per ml, motility 49.0% and forward progression 2.3. No differences in semen parameters were observed during greater than 1 year of followup. No impact on semen parameters was observed as a function of testosterone formulation. No patient became azoospermic during concomitant testosterone replacement and human chorionic gonadotropin therapy. Nine of 26 men contributed to pregnancy with the partner during followup.
Conclusions: Low dose human chorionic gonadotropin appears to maintain semen parameters in hypogonadal men on testosterone replacement therapy. Concurrent testosterone replacement and human chorionic gonadotropin use may preserve fertility in hypogonadal males who desire fertility preservation while on testosterone replacement therapy.
**************************
Low-Dose Human Chorionic Gonadotropin Maintains Intratesticular Testosterone in Normal Men with Testosterone-Induced Gonadotropin Suppression
Coviello AD, et al. J Clin Endocrinol Metab. 2005.
Abstract
In previous studies of testicular biopsy tissue from healthy men, intratesticular testosterone (ITT) has been shown to be much higher than serum testosterone (T), suggesting that high ITT is needed relative to serum T for normal spermatogenesis in men. However, the quantitative relationship between ITT and spermatogenesis is not known. To begin to address this issue experimentally, we determined the dose-response relationship between human chorionic gonadotropin (hCG) and ITT to ascertain the minimum dose needed to maintain ITT in the normal range. Twenty-nine men with normal reproductive physiology were randomized to receive 200 mg T enanthate weekly in combination with either saline placebo or 125, 250, or 500 IU hCG every other day for 3 wk. ITT was assessed in testicular fluid obtained by percutaneous fine needle aspiration at baseline and at the end of treatment. Baseline serum T (14.1 nmol/liter) was 1.2% of ITT (1174 nmol/liter). LH and FSH were profoundly suppressed to 5% and 3% of baseline, respectively, and ITT was suppressed by 94% (1234 to 72 nmol/liter) in the T enanthate/placebo group. ITT increased linearly with increasing hCG dose (P < 0.001). Posttreatment ITT was 25% less than baseline in the 125 IU hCG group, 7% less than baseline in the 250 IU hCG group, and 26% greater than baseline in the 500 IU hCG group. These results demonstrate that relatively low dose hCG maintains ITT within the normal range in healthy men with gonadotropin suppression. Extensions of this study will allow determination of the ITT concentration threshold required to maintain spermatogenesis in man.
MORE ON HCG:
The Use of HCG to Prevent / Reverse Testicular Shrinkage and Preserve Fertility
The use of human chorionic gonadotropin (hCG) in combination with testosterone replacement therapy (TRT) is a strategic approach to preserve fertility in men undergoing TRT, particularly those with hypogonadism. The effectiveness of hCG in this context is primarily due to its ability to mimic luteinizing hormone (LH), thereby stimulating intratesticular testosterone production, which is crucial for spermatogenesis.
### Effective Dosing of hCG
The most effective dose of hCG to preserve fertility while on TRT varies, but several studies provide guidance on dosing strategies that balance efficacy with minimizing potential side effects:
1. **Low-Dose hCG**: A common approach involves the administration of low-dose hCG to maintain intratesticular testosterone levels. Studies suggest that doses as low as 250 to 500 IU of hCG administered every other day can be effective. For instance, a study by Coviello et al. demonstrated that 500 IU hCG every other day maintained intratesticular testosterone within the normal range in healthy men with testosterone-induced gonadotropin suppression[19].
2. **Dose-Response Relationship**: Research indicates a dose-dependent response in intratesticular testosterone levels with varying doses of hCG. For example, a study found that increasing doses of hCG from 250 IU to 500 IU every other day resulted in higher intratesticular testosterone levels, suggesting that adjusting the dose based on individual response might be necessary[19].
3. **Combination with Clomiphene Citrate**: Some protocols recommend combining hCG with clomiphene citrate, another agent that stimulates endogenous testosterone production through a different mechanism. This combination can be particularly useful when trying to optimize fertility preservation[15].
4. **Monitoring and Adjustment**: It is crucial to monitor serum testosterone and intratesticular testosterone levels as well as sperm parameters to adjust hCG dosing appropriately. This ensures that the dose is sufficient to maintain spermatogenesis without causing supra-physiological testosterone levels that could have adverse effects[19].
### Clinical Recommendations
- **Starting Dose**: A typical starting dose can be around 500 IU every other day, with adjustments based on individual response and laboratory values[19].
- **Follow-Up**: Regular follow-up with semen analysis and hormone levels is recommended to ensure that the hCG dose is effectively maintaining fertility while on TRT[20].
- **Higher Doses**: In some cases, higher doses of hCG, ranging from 1500 IU to 3000 IU administered two to three times per week, might be used, especially in men with more severe hypogonadotropic hypogonadism[14].
### Conclusion
The effective dose of hCG for fertility preservation in men on TRT needs to be individualized based on the patient's response and hormonal levels. Low-dose hCG (250-500 IU every other day) is commonly effective, but doses may need to be adjusted based on the specific needs and responses of the individual. Regular monitoring of fertility parameters and hormone levels is essential to optimize treatment outcomes.
Sources
[1] TRT and Fertility - The Truth | Optimale https://www.optimale.co.uk/trt-uk/trt-and-fertility/
[2] a hypothesis on fertility optimization in men with hypergonadotrophic ... New frontiers in fertility preservation: a hypothesis on fertility optimization in men with hypergonadotrophic hypogonadism - Herati - Translational Andrology and Urology
[3] Preserving fertility in the hypogonadal patient: an update - PubMed Preserving fertility in the hypogonadal patient: an update - PubMed
[4] The Benefits of Using HCG with TRT - The Men's Health Clinic The Benefits of Using HCG with TRT - The Men’s Health Clinic
[5] Recovery of spermatogenesis following testosterone replacement ... Recovery of spermatogenesis following testosterone replacement therapy or anabolic-androgenic steroid use
[6] Reasons to Use hCG with TRT - Balance My Hormones Reasons to Use hCG with TRT - Balance My Hormones
[7] Low-dose hCG can prevent sterility in men prescribed testosterone Low-dose hCG can prevent sterility in men prescribed testosterone
[8] Testicular responses to hCG stimulation at varying doses in men ... Testicular responses to hCG stimulation at varying doses in men with spinal cord injury - Spinal Cord
[9] How to Decrease Infertility Risk While On TRT - Alpha Hormones How To Decrease Infertility Risk While On Testosterone Replacement Therapy Alpha Hormones
[10] Efficacy and Safety of Human Chorionic Gonadotropin Monotherapy ... Efficacy and Safety of Human Chorionic Gonadotropin Monotherapy for Men With Hypogonadal Symptoms and Normal Testosterone
[11] New frontiers in fertility preservation: a hypothesis on fertility ... - NCBI New frontiers in fertility preservation: a hypothesis on fertility optimization in men with hypergonadotrophic hypogonadism
[12] Indications for the use of human chorionic gonadotropic hormone for ... Indications for the use of human chorionic gonadotropic hormone for the management of infertility in hypogonadal men - Lee - Translational Andrology and Urology
[13] [PDF] Concomitant Intramuscular Human Chorionic Gonadotropin ... https://citeseerx.ist.psu.edu/docum...009beaa84f17e1fb171a603f3&repid=rep1&type=pdf
[14] Management of Male Fertility in Hypogonadal Patients on ... - MDPI Management of Male Fertility in Hypogonadal Patients on Testosterone Replacement Therapy
[15] Evaluating the Combination of Human Chorionic Gonadotropin and ... Evaluating the Combination of Human Chorionic Gonadotropin and Clomiphene Citrate in Treatment of Male Hypogonadotropic Hypogonadism: A Prospective Study
[16] Human Chorionic Gonadotropin (hCG) Injections for Men - Healthline Your Guide to Human Chorionic Gonadotropin (hCG) Injections for Men
[17] Dose-Dependent Increase in Intratesticular Testosterone by Very ... Dose-Dependent Increase in Intratesticular Testosterone by Very Low-Dose Human Chorionic Gonadotropin in Normal Men with Experimental Gonadotropin Deficiency
[18] HCG / Human Chorionic Gonadotropin for Male Infertility HCG / Human Chorionic Gonadotropin for Male Infertility — Male Infertility Guide
[19] Low-Dose Human Chorionic Gonadotropin Maintains Intratesticular ... Low-Dose Human Chorionic Gonadotropin Maintains Intratesticular Testosterone in Normal Men with Testosterone-Induced Gonadotropin Suppression
[20] Low dose human chorionic gonadotropin prevents azoospermia and ... https://www.fertstert.org/article/S0015-0282(10)01624-9/fulltext
Last edited:
















