Nelson Vergel
Founder, ExcelMale.com
Dr Saya:
You know how much I like data even if it is from a small pilot or case study. Thanks for this!
I was able to paste the text here to make it easier for people to read:
Serum Beta hCG Concentrations Resulting from Single hCG Injection
Dr Justin Saya, M.D. Defy Medical, LLC
Prior to delving into discussion, I wanted to take time to express a special thank you to Defy Medical management and staff for following through with the logistics of the following case study, the study participants for their willingness to volunteer, and also my colleagues, Jill Dillenburg, RN and Dr John Crisler, D.O. for their support of the case study.
Introduction
The human endocrine system comprises a complex network of organs, glands, hormones, receptors, binding globulins, enzymes, and mRNA/DNA transcription cascades that result in a multitude of vital end-products and processes throughout the body. Furthermore, this network is, for the most part, self-regulating via intricate control processes involving both positive and negative feedback loops.
One such negative feedback loop is particularly relevant for male patients prescribed treatment for hypogonadism with testosterone replacement therapy. The introduction of exogenous testosterone into the endocrine system initiates a negative feedback loop whereby endogenous testosterone production is suppressed/halted via suppression of the hypothalamus-pituitary signaling resulting in a steep decline (and eventual cessation) of luteinizing hormone (LH) production. Of note, introduction of exogenous testosterone also suppresses the pituitary production of another gonadotropin, follicle stimulating hormone (FSH), however we will focus on luteinizing hormone for this discussion as it relates to human chorionic gonadotropin (hCG). The physiologic action of luteinizing hormone in the male body is to stimulate the leydig cells of the testes (for testosterone production). Thus, with the introduction of exogenous testosterone for a male on testosterone replacement therapy, and the resultant suppression of endogenous luteinizing hormone (LH) and follicle stimulating hormone (FSH), the testes go without stimulation and will become inactive (dormant). The consequence of this inactivity of the testes is a significant decline in fertility/spermatogenesis, decline in endogenous testicular testosterone production, and often atrophy (shrinkage) of the testes.
Human chorionic gonadotropin (hCG) has been shown to be an analog of endogenous luteinizing hormone. Human chorionic gonadotropin is so similar in structure to endogenous luteinizing hormone, in fact, that hCG interacts with the luteinizing hormone receptors on the testicular leydig cells and will stimulate their activity. Thus, hCG has been shown both clinically and scientifically to reverse signs and symptoms of testicular suppression for males on testosterone replacement.
Indeed, introduction of hCG for a male on testosterone replacement therapy whom has experienced suppression of the testes, will often improve spermatogenesis, testicular fullness/volume, and endogenous testicular testosterone production.
Given the growing awareness of the benefits of hCG treatment as an adjunct to TRT for male patients, the use of hCG has been increasing significantly. However, despite the increase in use, there has been no consensus reached regarding the ideal or optimal dosing. This article will not attempt to establish concrete recommendations for ideal dosing regimens, but, rather, will outline a case study of serum hCG concentrations achieved during a 72 hour period immediately following a single hCG injection of 150iu and 500iu in two test subjects. As the goal of adjunctive hCG treatment is to mimic the action (and amplitude) of the lost luteinizing hormone stimulation, it is my position that hCG dosing guidelines should be designed for exactly this purpose. In other words, dosing guidelines should aim to, as closely as possible, mimic the endogenous action and amplitude of luteinizing hormone stimulation, with care taken to avoid both under-stimulating or over-stimulating in comparison to endogenous luteinizing hormone levels.
Laboratory studies for both luteinizing hormone and beta hCG concentrations are reported in the same units (mIU/mL), making comparison, at least in this regard, fairly straightforward. However, discussion will be made regarding the varying half-life and pattern of secretion of endogenous luteinizing hormone and injected human chorionic gonadotropin. Luteinizing hormone is secreted in a pulsatile nature from the pituitary gland with a half-life estimated at approximately 20 minutes. On the contrary, hCG is injected, not secreted in pulses, and has a much longer half-life estimated at approximately 24-30 hours. As a consequence, the “area under the curve” (AUC) and resultant biological potency for these two differs distinctly.
Methods
This small case study is comprised of two test subjects, a 34 year-old male and a 47 year-old male, both of which have been on testosterone replacement therapy for greater than a five year duration, and both of which were verified and documented to have suppressed endogenous luteinizing hormone levels (0.1) prior to commencement of the study. This is significant as the laboratory methodology for serum beta hCG quantitative testing is Roche ECLIA, with possible cross- reactivity for the serum hCG test via endogenous luteinizing hormone. However, verifying absent endogenous luteinizing hormone levels (0.1 – lowest value for lab result) for the test subjects eliminates the possibility of this cross-reactivity skewing the study results. Both patients were previously on hCG treatment as an adjunct to their TRT, however their hCG treatment was ceased 7 days prior to study commencement as a wash-out period, and baseline serum hCG levels were confirmed to be <1 (lowest threshold for lab results, in effect 0) immediately prior to the single hCG injection to commence the study.
The 34 year-old subject (subject “A”) had serum luteinizing hormone and quantitative serum beta hCG concentrations tested at hour 0 (prior to single hCG injection), then a single hCG injection of 150iu subcutaneously was administered, with subsequent quantitative serum beta hCG concentrations drawn at hour 8, hour 24, hour 48, and hour 72 following the 150iu injection. The 47 year-old subject (subject “B”) had serum luteinizing hormone and quantitative serum beta hCG concentrations tested at hour 0 (prior to single hCG injection), then a single hCG injection of 500iu subcutaneously was administered, with subsequent quantitative serum beta hCG concentrations drawn at hour 8, hour 24, hour 48, and hour 72 following the 500iu injection. Each subject was injected from a vial of freshly reconstituted hCG, kept under favorable conditions and refrigerated throughout duration of study, and both subjects were injected with hCG from the same vial to avoid possible vial-to-vial variability.
Results
Results for both subject A and subject B for the serum tests at hour 0 (after 7 day wash-out with no hCG and before the single test hCG injection) demonstrated serum luteinizing hormone level 0.1 mIU/mL (lower threshold for results, in effect 0) for both test subjects, and quantitative serum beta hCG level <1 mIU/mL (lower threshold for results, in effect 0) for both test subjects. Results of the quantitative serum beta hCG concentration tests administered at hour 0, hour 8, hour 24, hour 48, and hour 72 are summarized in Table 1 below.
Table 1
Quantitative serum beta hCG concentration - hour 0, hour 8, hour 24, hour 48, hour 72
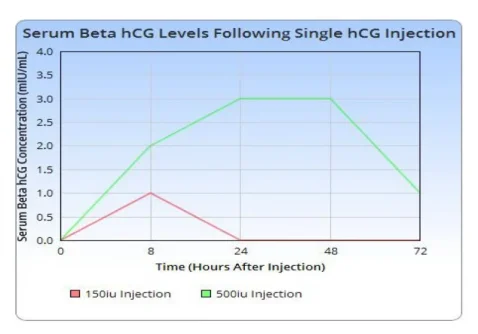
A graphical representation of the resultant quantitative serum beta hCG concentrations is depicted below in Graph 1.
Graph 1
Quantitative serum beta hCG concentration - hour 0, hour 8, hour 24, hour 48, hour 72
View attachment 1768
A relevant note for consideration in comparison of quantitative serum beta hCG concentrations with endogenous luteinizing hormone (LH) concentrations is that the typical “normal” range for endogenous LH is 1.7 – 8.6 mIU/mL. As noted, half-life differences (of large magnitude) are present, but this offers some perspective with the comparison.
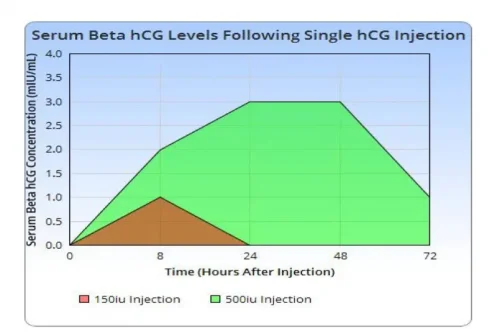
A graphical representation of the resultant quantitative serum beta hCG concentrations with shading to demonstrate area under curve is depicted below in Graph 2.
Graph 2
Shading of Area Under Curve
Quantitative serum beta hCG concentration - hour 0, hour 8, hour 24, hour 48, hour 72
View attachment 1769
Discussion
This data indicates that there is indeed a drastic difference in quantitative serum beta hCG concentrations achieved following a single hCG injection of 150iu vs 500iu. More interesting is the fact that this dose-response relationship does NOT appear to be linear based on this limited data. The serum beta hCG concentration following a single hCG injection of 150iu appears to peak at ~1mIU/mL at 8 hours and has retreated to baseline prior to 24 hours after the injection. On the contrary, the serum beta hCG concentration following a single hCG injection of 500iu attains a level of 2mIU/mL at 8 hours and subsequently INCREASES to 3mIU/mL at 24 hours and 48 hours, before retreating to 1mIU/mL at 72 hours (still has not declined to baseline <1 by the 72 hour mark following injection). Taking into account the physiologic range of luteinizing hormone (LH) of 1.7 – 8.6mIU/mL (and once again the differences in half-life) can enable some interesting debate on the physiologic/biological effects of these resultant levels. Further, the apparent time to retreat to baseline levels can offer some guidance on dosing frequency/timing for these varying dosages of hCG.
According to this data, it would appear that a hCG dosage of 150iu would have to be administered on AT LEAST a daily basis (if not more frequently) to allow continual stimulation of the leydig cells of the testes. Further, with an apparent maximal serum concentration from a hCG dosage of 150iu reaching a peak of ~1mIU/mL, this may prove to be insufficient stimulation for SOME patients to achieve consistent testicular activity and prevent the aforementioned side effects of testicular deactivation/dormancy. Certainly one could debate the relative need for continual stimulation of the testes, however this may offer a clue for dosage adjustments for patients that either experience poor results, poor fertility, or continued decrease in testicular volume at lower hCG dosages.
A single dosage of 500iu of hCG appears to exert a much more prolonged (and pronounced) increase in serum beta hCG concentrations, likely coinciding with a more prolonged and pronounced biological effect. Once again, whether this is beneficial or detrimental, can certainly be debated and will often hinge on many factors on an individualized case by case basis. It does appear obvious from the data that a dosage of 500iu of hCG will maintain levels >1mIU/mL for up to 3 days (72 hours) following a single injection. Thus, it would seem a direct conclusion to state that an hCG injection of 500iu every 3.5 days (twice weekly) would provide relatively continual stimulation of the leydig cells of the testes (concentration >1mIU/mL), and injections of this magnitude in dosage would NOT be needed any more frequently than that.
My clinical mind and instincts suggest that the “ideal” hCG dosage likely lies in between these two extremes (150iu vs 500iu) and ideal frequency will hinge upon ideal dosage (with 150iu or less dosages likely requiring daily or even more frequent injections) and larger dosages (500iu, possibly even slightly smaller) requiring no more frequent than twice weekly injections, but this conclusion simply cannot be made concretely from this limited data. Furthermore, dosage decisions and frequencies are always individualized case-by-case based on many variables specific to the individual (fertility considerations, injection compliance, complicating factors such as SHBG levels, current/prior response to hCG, estradiol levels, testicular health, etc). Without specific data on other dosages (which I would like to obtain), these patterns suggest that a dosage regimen of hCG 250iu-350iu on an every other day (QOD) schedule would likely offer an alternative regimen for relatively steady and consistent testicular stimulation, although these conclusions are only speculative and cannot be drawn definitively from this limited data.
Conclusions
The clinical use of human chorionic gonadotropin (hCG) as an adjunctive treatment to testosterone replacement therapy (TRT) in males is an important, and often overlooked and misunderstood, aspect of successful treatment of hypogonadism. However, a consensus on use and dosing/frequency has not been reached among practitioners and the situation is complicated by the degree of bio-hormonal individuality present across the population and the varying effects and goals of hCG treatment in different clinical scenarios (low SHBG levels, high estradiol levels, fertility concerns, etc). The data in this limited case study suggest that a dosage of 150iu hCG appears to attain minimal to moderate stimulation (serum concentration of 1mIU/mL) of the testicular leydig cells for a duration less than 24 hours and would likely be insufficient to attain continuous stimulation of the testicular leydig cells, UNLESS given on a daily basis, perhaps more frequently. Whereas, an injection of hCG 500iu appears to attain moderate stimulation (serum concentration 2mIU/mL -> 3mIU/mL -> 3mIU/mL -> 1mIU/mL) for a period slightly longer than
3 days (72 hours), likely enabling twice weekly, evenly spread, injections to attain continuous stimulation. As noted previously, I believe these patterns also suggest that a dosage regimen of hCG 250iu-350iu on an every other day (QOD) schedule would likely offer an alternative regimen for moderate, relatively steady and consistent testicular stimulation, although more data would be needed to confirm this conclusion.
As a future consideration, and to offer more insight, I would like to obtain data on dosages between 150iu and 500iu, specifically 250iu and 350iu dosages. Further, the apparent non-linear dose response relationship in this data is intriguing and would warrant further study. Due to the interesting serum results within the first 24 hour period from the smaller 150iu hCG dosage and the logistical limitations in this study of obtaining results at 8 hours and then 24 hours, it would be useful to obtain data on serum hCG concentrations at several time points WITHIN the first 24 hour period, especially following smaller hCG dosages (150iu or less). Indeed, further study would assist in shedding more light onto the preferred dosage and frequency suggestions for hCG use as an adjunct to TRT in male patients and continue the advancement of this treatment into mainstream usage.
You know how much I like data even if it is from a small pilot or case study. Thanks for this!
I was able to paste the text here to make it easier for people to read:
Serum Beta hCG Concentrations Resulting from Single hCG Injection
Dr Justin Saya, M.D. Defy Medical, LLC
Prior to delving into discussion, I wanted to take time to express a special thank you to Defy Medical management and staff for following through with the logistics of the following case study, the study participants for their willingness to volunteer, and also my colleagues, Jill Dillenburg, RN and Dr John Crisler, D.O. for their support of the case study.
Introduction
The human endocrine system comprises a complex network of organs, glands, hormones, receptors, binding globulins, enzymes, and mRNA/DNA transcription cascades that result in a multitude of vital end-products and processes throughout the body. Furthermore, this network is, for the most part, self-regulating via intricate control processes involving both positive and negative feedback loops.
One such negative feedback loop is particularly relevant for male patients prescribed treatment for hypogonadism with testosterone replacement therapy. The introduction of exogenous testosterone into the endocrine system initiates a negative feedback loop whereby endogenous testosterone production is suppressed/halted via suppression of the hypothalamus-pituitary signaling resulting in a steep decline (and eventual cessation) of luteinizing hormone (LH) production. Of note, introduction of exogenous testosterone also suppresses the pituitary production of another gonadotropin, follicle stimulating hormone (FSH), however we will focus on luteinizing hormone for this discussion as it relates to human chorionic gonadotropin (hCG). The physiologic action of luteinizing hormone in the male body is to stimulate the leydig cells of the testes (for testosterone production). Thus, with the introduction of exogenous testosterone for a male on testosterone replacement therapy, and the resultant suppression of endogenous luteinizing hormone (LH) and follicle stimulating hormone (FSH), the testes go without stimulation and will become inactive (dormant). The consequence of this inactivity of the testes is a significant decline in fertility/spermatogenesis, decline in endogenous testicular testosterone production, and often atrophy (shrinkage) of the testes.
Human chorionic gonadotropin (hCG) has been shown to be an analog of endogenous luteinizing hormone. Human chorionic gonadotropin is so similar in structure to endogenous luteinizing hormone, in fact, that hCG interacts with the luteinizing hormone receptors on the testicular leydig cells and will stimulate their activity. Thus, hCG has been shown both clinically and scientifically to reverse signs and symptoms of testicular suppression for males on testosterone replacement.
Indeed, introduction of hCG for a male on testosterone replacement therapy whom has experienced suppression of the testes, will often improve spermatogenesis, testicular fullness/volume, and endogenous testicular testosterone production.
Given the growing awareness of the benefits of hCG treatment as an adjunct to TRT for male patients, the use of hCG has been increasing significantly. However, despite the increase in use, there has been no consensus reached regarding the ideal or optimal dosing. This article will not attempt to establish concrete recommendations for ideal dosing regimens, but, rather, will outline a case study of serum hCG concentrations achieved during a 72 hour period immediately following a single hCG injection of 150iu and 500iu in two test subjects. As the goal of adjunctive hCG treatment is to mimic the action (and amplitude) of the lost luteinizing hormone stimulation, it is my position that hCG dosing guidelines should be designed for exactly this purpose. In other words, dosing guidelines should aim to, as closely as possible, mimic the endogenous action and amplitude of luteinizing hormone stimulation, with care taken to avoid both under-stimulating or over-stimulating in comparison to endogenous luteinizing hormone levels.
Laboratory studies for both luteinizing hormone and beta hCG concentrations are reported in the same units (mIU/mL), making comparison, at least in this regard, fairly straightforward. However, discussion will be made regarding the varying half-life and pattern of secretion of endogenous luteinizing hormone and injected human chorionic gonadotropin. Luteinizing hormone is secreted in a pulsatile nature from the pituitary gland with a half-life estimated at approximately 20 minutes. On the contrary, hCG is injected, not secreted in pulses, and has a much longer half-life estimated at approximately 24-30 hours. As a consequence, the “area under the curve” (AUC) and resultant biological potency for these two differs distinctly.
Methods
This small case study is comprised of two test subjects, a 34 year-old male and a 47 year-old male, both of which have been on testosterone replacement therapy for greater than a five year duration, and both of which were verified and documented to have suppressed endogenous luteinizing hormone levels (0.1) prior to commencement of the study. This is significant as the laboratory methodology for serum beta hCG quantitative testing is Roche ECLIA, with possible cross- reactivity for the serum hCG test via endogenous luteinizing hormone. However, verifying absent endogenous luteinizing hormone levels (0.1 – lowest value for lab result) for the test subjects eliminates the possibility of this cross-reactivity skewing the study results. Both patients were previously on hCG treatment as an adjunct to their TRT, however their hCG treatment was ceased 7 days prior to study commencement as a wash-out period, and baseline serum hCG levels were confirmed to be <1 (lowest threshold for lab results, in effect 0) immediately prior to the single hCG injection to commence the study.
The 34 year-old subject (subject “A”) had serum luteinizing hormone and quantitative serum beta hCG concentrations tested at hour 0 (prior to single hCG injection), then a single hCG injection of 150iu subcutaneously was administered, with subsequent quantitative serum beta hCG concentrations drawn at hour 8, hour 24, hour 48, and hour 72 following the 150iu injection. The 47 year-old subject (subject “B”) had serum luteinizing hormone and quantitative serum beta hCG concentrations tested at hour 0 (prior to single hCG injection), then a single hCG injection of 500iu subcutaneously was administered, with subsequent quantitative serum beta hCG concentrations drawn at hour 8, hour 24, hour 48, and hour 72 following the 500iu injection. Each subject was injected from a vial of freshly reconstituted hCG, kept under favorable conditions and refrigerated throughout duration of study, and both subjects were injected with hCG from the same vial to avoid possible vial-to-vial variability.
Results
Results for both subject A and subject B for the serum tests at hour 0 (after 7 day wash-out with no hCG and before the single test hCG injection) demonstrated serum luteinizing hormone level 0.1 mIU/mL (lower threshold for results, in effect 0) for both test subjects, and quantitative serum beta hCG level <1 mIU/mL (lower threshold for results, in effect 0) for both test subjects. Results of the quantitative serum beta hCG concentration tests administered at hour 0, hour 8, hour 24, hour 48, and hour 72 are summarized in Table 1 below.
Table 1
Quantitative serum beta hCG concentration - hour 0, hour 8, hour 24, hour 48, hour 72
| Hours after hCG Injection | Serum hCG Concentration (mIU/mL) 150iu Injection | Serum hCG Concentration (mIU/mL) 500iu Injection |
| 0 | 0 | 0 |
| 8 | 1 | 2 |
| 24 | 0 | 3 |
| 48 | 0 | 3 |
| 72 | 0 | 1 |
A graphical representation of the resultant quantitative serum beta hCG concentrations is depicted below in Graph 1.
Graph 1
Quantitative serum beta hCG concentration - hour 0, hour 8, hour 24, hour 48, hour 72
View attachment 1768
A relevant note for consideration in comparison of quantitative serum beta hCG concentrations with endogenous luteinizing hormone (LH) concentrations is that the typical “normal” range for endogenous LH is 1.7 – 8.6 mIU/mL. As noted, half-life differences (of large magnitude) are present, but this offers some perspective with the comparison.
A graphical representation of the resultant quantitative serum beta hCG concentrations with shading to demonstrate area under curve is depicted below in Graph 2.
Graph 2
Shading of Area Under Curve
Quantitative serum beta hCG concentration - hour 0, hour 8, hour 24, hour 48, hour 72
View attachment 1769
Discussion
This data indicates that there is indeed a drastic difference in quantitative serum beta hCG concentrations achieved following a single hCG injection of 150iu vs 500iu. More interesting is the fact that this dose-response relationship does NOT appear to be linear based on this limited data. The serum beta hCG concentration following a single hCG injection of 150iu appears to peak at ~1mIU/mL at 8 hours and has retreated to baseline prior to 24 hours after the injection. On the contrary, the serum beta hCG concentration following a single hCG injection of 500iu attains a level of 2mIU/mL at 8 hours and subsequently INCREASES to 3mIU/mL at 24 hours and 48 hours, before retreating to 1mIU/mL at 72 hours (still has not declined to baseline <1 by the 72 hour mark following injection). Taking into account the physiologic range of luteinizing hormone (LH) of 1.7 – 8.6mIU/mL (and once again the differences in half-life) can enable some interesting debate on the physiologic/biological effects of these resultant levels. Further, the apparent time to retreat to baseline levels can offer some guidance on dosing frequency/timing for these varying dosages of hCG.
According to this data, it would appear that a hCG dosage of 150iu would have to be administered on AT LEAST a daily basis (if not more frequently) to allow continual stimulation of the leydig cells of the testes. Further, with an apparent maximal serum concentration from a hCG dosage of 150iu reaching a peak of ~1mIU/mL, this may prove to be insufficient stimulation for SOME patients to achieve consistent testicular activity and prevent the aforementioned side effects of testicular deactivation/dormancy. Certainly one could debate the relative need for continual stimulation of the testes, however this may offer a clue for dosage adjustments for patients that either experience poor results, poor fertility, or continued decrease in testicular volume at lower hCG dosages.
A single dosage of 500iu of hCG appears to exert a much more prolonged (and pronounced) increase in serum beta hCG concentrations, likely coinciding with a more prolonged and pronounced biological effect. Once again, whether this is beneficial or detrimental, can certainly be debated and will often hinge on many factors on an individualized case by case basis. It does appear obvious from the data that a dosage of 500iu of hCG will maintain levels >1mIU/mL for up to 3 days (72 hours) following a single injection. Thus, it would seem a direct conclusion to state that an hCG injection of 500iu every 3.5 days (twice weekly) would provide relatively continual stimulation of the leydig cells of the testes (concentration >1mIU/mL), and injections of this magnitude in dosage would NOT be needed any more frequently than that.
My clinical mind and instincts suggest that the “ideal” hCG dosage likely lies in between these two extremes (150iu vs 500iu) and ideal frequency will hinge upon ideal dosage (with 150iu or less dosages likely requiring daily or even more frequent injections) and larger dosages (500iu, possibly even slightly smaller) requiring no more frequent than twice weekly injections, but this conclusion simply cannot be made concretely from this limited data. Furthermore, dosage decisions and frequencies are always individualized case-by-case based on many variables specific to the individual (fertility considerations, injection compliance, complicating factors such as SHBG levels, current/prior response to hCG, estradiol levels, testicular health, etc). Without specific data on other dosages (which I would like to obtain), these patterns suggest that a dosage regimen of hCG 250iu-350iu on an every other day (QOD) schedule would likely offer an alternative regimen for relatively steady and consistent testicular stimulation, although these conclusions are only speculative and cannot be drawn definitively from this limited data.
Conclusions
The clinical use of human chorionic gonadotropin (hCG) as an adjunctive treatment to testosterone replacement therapy (TRT) in males is an important, and often overlooked and misunderstood, aspect of successful treatment of hypogonadism. However, a consensus on use and dosing/frequency has not been reached among practitioners and the situation is complicated by the degree of bio-hormonal individuality present across the population and the varying effects and goals of hCG treatment in different clinical scenarios (low SHBG levels, high estradiol levels, fertility concerns, etc). The data in this limited case study suggest that a dosage of 150iu hCG appears to attain minimal to moderate stimulation (serum concentration of 1mIU/mL) of the testicular leydig cells for a duration less than 24 hours and would likely be insufficient to attain continuous stimulation of the testicular leydig cells, UNLESS given on a daily basis, perhaps more frequently. Whereas, an injection of hCG 500iu appears to attain moderate stimulation (serum concentration 2mIU/mL -> 3mIU/mL -> 3mIU/mL -> 1mIU/mL) for a period slightly longer than
3 days (72 hours), likely enabling twice weekly, evenly spread, injections to attain continuous stimulation. As noted previously, I believe these patterns also suggest that a dosage regimen of hCG 250iu-350iu on an every other day (QOD) schedule would likely offer an alternative regimen for moderate, relatively steady and consistent testicular stimulation, although more data would be needed to confirm this conclusion.
As a future consideration, and to offer more insight, I would like to obtain data on dosages between 150iu and 500iu, specifically 250iu and 350iu dosages. Further, the apparent non-linear dose response relationship in this data is intriguing and would warrant further study. Due to the interesting serum results within the first 24 hour period from the smaller 150iu hCG dosage and the logistical limitations in this study of obtaining results at 8 hours and then 24 hours, it would be useful to obtain data on serum hCG concentrations at several time points WITHIN the first 24 hour period, especially following smaller hCG dosages (150iu or less). Indeed, further study would assist in shedding more light onto the preferred dosage and frequency suggestions for hCG use as an adjunct to TRT in male patients and continue the advancement of this treatment into mainstream usage.