Nelson Vergel
Founder, ExcelMale.com
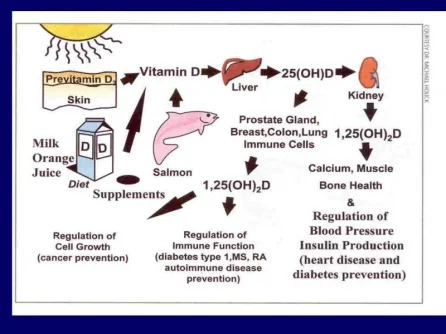
Vitamin D is responsible for enhancing intestinal absorption of calcium, iron, magnesium, phosphate and zinc. In humans, the most important compounds in this group are vitamin D3 (also known as cholecalciferol) and vitamin D2 (ergocalciferol). Cholecalciferol and ergocalciferol can be ingested from the diet and from supplements. The body can also synthesize vitamin D (specifically cholecalciferol) in the skin, from cholesterol, when sun exposure is adequate.
To attempt to minimize vitamin deficiency due to low sunshine exposure or vitamin D intake, vitamin D is added to staple foods such as milk, cereals, orange juice, etc. Cold water fish is also rich in vitamin D (salmon and others). Because of uncertainty about the skin cancer risk from sunlight, no recommendations are issued by the Institute of Medicine for the amount of sun exposure required to meet vitamin D requirements. Accordingly, the Dietary Reference Intake for vitamin D assumes no synthesis occurs and all of a person's vitamin D is from food intake, although that will rarely occur in practice.
Beyond its use to prevent bone loss, the evidence for other health effects of vitamin D supplementation in the general population is inconsistent. The effect of vitamin D supplementation on mortality is not clear, with one meta-analysis finding a decrease in mortality in elderly people, and another concluding there is no clear justification for recommending vitamin D.
Vitamin D synthesis may be lower in people with darker skin, obese patients, those who do not consume enough sources of vitamin D or get enough sun exposure. We all have lower vitamin D levels in winter months when there is less sunshine. Also, some medications may interfere with how vitamin D gets metabolized.
Some studies show that for most white people, a half-hour in the summer sun in a bathing suit can initiate the release of 50,000 IU (1.25 mg) vitamin D into the circulation within 24 hours of exposure; this same amount of exposure yields 20,000–30,000 IU in tanned individuals and 8,000–10,000 IU in dark-skinned people.
The 25-hydroxy vitamin D test is the most accurate way to measure how much vitamin D is in your body.In the kidney, 25-hydroxy vitamin D changes into an active form of the vitamin. The active form of vitamin D helps control calcium and phosphate levels in the body. The normal range is 30.0 to 74.0 nanograms per milliliter (ng/mL).
There is speculation that high vitamin D doses may increase the risk of kidney stones. However, "most of the observational studies do not support a significant association between higher nutritional vitamin D store and increased risk of stone formation. Short-term nutritional vitamin D repletion in stone formers with vitamin D deficiency also does not appear to increase urinary calcium excretion."
Vitamin D deficiency is common among HIV-infected persons throughout the world, with prevalence estimates ranging widely from 29% to 87%. It has been associated with faster disease progression and higher mortality and greater prevalence of diabetes. In two recent studies of HIV-infected subjects, low vitamin D concentrations were associated with increased carotid intima-media thickness, a measure of subclinical atherosclerosis. One randomized trial has demonstrated the safety and effectiveness of oral cholecalciferol (vitamin D3) in HIV-infected adolescents; however, no randomized placebo-controlled trials have been conducted in adults.
The study done in adolescents living with HIV showed that Vitamin D supplementation (an oral dose of 50,000-unit once per month for 3 months) may help prevent hormonal changes that can lead to bone loss among those being treated for HIV with tenofovir (found in Viread, Truvada and Atripla) . However, the drug causes symptoms that resemble those of vitamin D deficiency, causing bones to lose calcium and reducing bone density.
The study found that large monthly doses of vitamin D reduced blood levels of parathyroid hormone, an endocrine regulator that stimulates calcium release from bones, potentially weakening them and causing them to break more easily. Normally, when the body is deficient in vitamin D, parathyroid hormone levels increase. Parathyroid hormone also tends to be elevated in people taking tenofovir, whether or not they have sufficient vitamin D.
Another small study published on Antiviral Therapy (2012) showed that giving 45 adult HIV+ patients with low blood levels of vitamin D a dose of 4000 units of vitamin D3 per day for 12 weeks modestly improved vitamin D status and cholesterol but worsened insulin resistance without change in endothelial function (blood vessels did not dilate to improve blood flow). The most striking finding is that many patients taking this dose failed to achieve normal Vitamin D blood levels as shown by its metabolite 25(OH)D.
The Endocrine Society has published guidelines that recommend screening for vitamin D deficiency in all HIV-infected patients on antiretroviral therapy since some HIV medications may potentially affect vitamin D metabolism . More specifically, the antiretroviral drug efavirenz (EFV) has been associated with vitamin D deficiency in recent cross-sectional studies . Initiation of EFV lowered 25(OH)D concentrations in two prospective studies , and switching from EFV to a protease inhibitor based regimen raised 25(OH)D concentrations in the MONET trial. The effect of EFV on active vitamin D supplementation is, however, unknown.
Here is a list of vitamin D studies currently enrolling HIV+ people:
[TABLE="class: data_table margin-top, width: 934"]
[TR]
[TD="align: center"]1[/TD]
[TD="align: center"]Recruiting[/TD]
[TD]Vitamin D HIV Study[TABLE="class: data_table body3"]
[TR]
[TH="align: right"]Condition:[/TH]
[TD]HIV[/TD]
[/TR]
[TR]
[TH="align: right"]Interventions:[/TH]
[TD]Drug: Vitamin D3; Drug: Placebo[/TD]
[/TR]
[/TABLE]
[/TD]
[/TR]
[TR]
[TD="align: center"]2[/TD]
[TD="align: center"]Recruiting[/TD]
[TD]Vitamin D Supplementation in HIV Youth[TABLE="class: data_table body3"]
[TR]
[TH="align: right"]Condition:[/TH]
[TD]HIV+[/TD]
[/TR]
[TR]
[TH="align: right"]Intervention:[/TH]
[TD]Drug: Vitamin D3[/TD]
[/TR]
[/TABLE]
[/TD]
[/TR]
[TR]
[TD="align: center"]3[/TD]
[TD="align: center"]Recruiting[/TD]
[TD]Bone Health and Vitamin D Status[TABLE="class: data_table body3"]
[TR]
[TH="align: right"]Conditions:[/TH]
[TD]Osteopenia; Vitamin D Deficiency; HIV Infection[/TD]
[/TR]
[TR]
[TH="align: right"]Intervention:[/TH]
[TD][/TD]
[/TR]
[/TABLE]
[/TD]
[/TR]
[TR]
[TD="align: center"]4[/TD]
[TD="align: center"]Recruiting[/TD]
[TD]Vitamin D Supplements for HIV-positive Patients on cART[TABLE="class: data_table body3"]
[TR]
[TH="align: right"]Condition:[/TH]
[TD]HIV-associated Co-morbidities[/TD]
[/TR]
[TR]
[TH="align: right"]Interventions:[/TH]
[TD]Dietary Supplement: conventional vitamin D treatment; Drug: tiered/titrated vitamin D dosing[/TD]
[/TR]
[/TABLE]
[/TD]
[/TR]
[TR]
[TD="align: center"]5[/TD]
[TD="align: center"]Unknown [SUP]†[/SUP][/TD]
[TD]The Prevalence of Vitamin D Deficiency and Effects of Vitamin D Supplementation in HIV-1 Infected Patients[TABLE="class: data_table body3"]
[TR]
[TH="align: right"]Conditions:[/TH]
[TD]Vitamin D Deficiency; HIV Infections[/TD]
[/TR]
[TR]
[TH="align: right"]Intervention:[/TH]
[TD]Drug: colecalciferol[/TD]
[/TR]
[/TABLE]
[/TD]
[/TR]
[TR]
[TD="align: center"]6[/TD]
[TD="align: center"]Recruiting[/TD]
[TD]Vit D and HIV-Cardiovascular Disease in Children and Young Adults Vitamin D and HIV-CVD in Children and Young Adults[TABLE="class: data_table body3"]
[TR]
[TH="align: right"]Condition:[/TH]
[TD]Vitamin D Deficiency[/TD]
[/TR]
[TR]
[TH="align: right"]Intervention:[/TH]
[TD][/TD]
[/TR]
[/TABLE]
[/TD]
[/TR]
[TR]
[TD="align: center"]7[/TD]
[TD="align: center"]Recruiting[/TD]
[TD]Immune Reconstitution in HIV Disease (IREHIV)[TABLE="class: data_table body3"]
[TR]
[TH="align: right"]Condition:[/TH]
[TD]HIV Infection[/TD]
[/TR]
[TR]
[TH="align: right"]Interventions:[/TH]
[TD]Drug: vitamin D (cholecalciferol) and PBA (sodium phenylbutyrate); Drug: Placebo tablets[/TD]
[/TR]
[/TABLE]
[/TD]
[/TR]
[TR]
[TD="align: center"]8[/TD]
[TD="align: center"]Recruiting[/TD]
[TD]Trial of Vitamin D in HIV Progression[TABLE="class: data_table body3"]
[TR]
[TH="align: right"]Condition:[/TH]
[TD]HIV Infection[/TD]
[/TR]
[TR]
[TH="align: right"]Interventions:[/TH]
[TD]Dietary Supplement: Vitamin D3 (cholecalciferol); Other: Placebo[/TD]
[/TR]
[/TABLE]
[/TD]
[/TR]
[TR]
[TD="align: center"]9[/TD]
[TD="align: center"]Recruiting[/TD]
[TD]Prevalence of Vertebral Fractures in HIV Infected Patients Older Than 50 Years[TABLE="class: data_table body3"]
[TR]
[TH="align: right"]Condition:[/TH]
[TD]Vertebral Fractures[/TD]
[/TR]
[TR]
[TH="align: right"]Intervention:[/TH]
[TD][/TD]
[/TR]
[/TABLE]
[/TD]
[/TR]
[/TABLE]
Last edited:














