madman
Super Moderator
* Electrical neurostimulation of the penis, they explain, targets the penile-nerve supply that may be impaired by disease, injury, or aging, thus promoting authentic nerve functioning. The authors argue that this approach may address limitations of existing treatments by acting as a restorative therapy rather than a compensatory one.
* “We are grateful to Dr. [Arthur] Burnett, and the other co-authors for advancing this work, which we believe will represent a cornerstone for the field of neurostimulation and erectile dysfunction management. By stimulating the cavernous nerves at a time when injury is predictable, we may be able to promote neural rehabilitation and facilitate functional recovery rather than accepting postoperative erectile dysfunction as inevitable. While larger controlled trials are required, the early data strongly support continued clinical investigation.”

Key Takeaways

 www.urologytimes.com
www.urologytimes.com
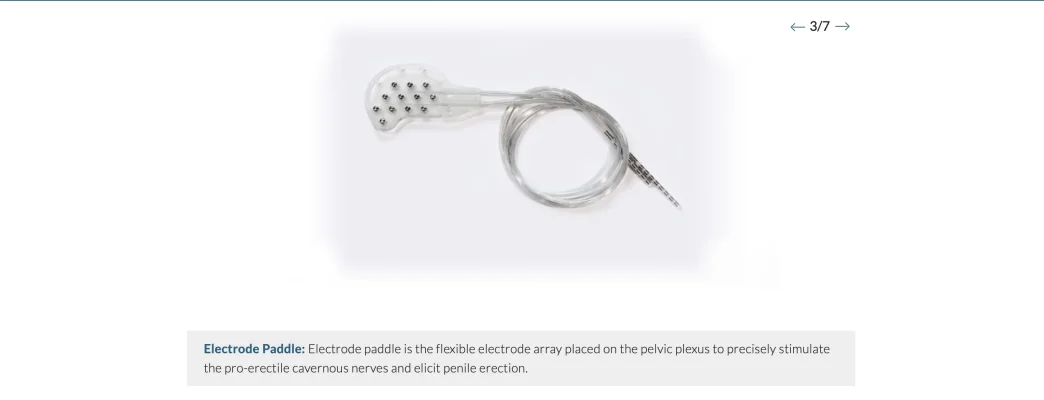
Data from a first-in-man clinical study (NCT05650866) of the CaverSTIM device have been published in BJU International, showing encouraging outcomes with the implantable cavernous nerve neurostimulator in restoring erectile function following robot-assisted radical prostatectomy (RARP).1
In addition to the early phase trial results, a review on the scientific rationale for using implantable neurostimulation was concurrently published in Nature Urology Review.2

Pim van Wesel
“These publications reflect a major step forward for CaverSTIM and for Comphya,” said Pim van Wesel, CEO of Comphya, in a news release from the company.2 “Seeing our technology validated in a first-in-man clinical study reinforces our confidence that neuromodulation can meaningfully improve quality-of-life outcomes for men undergoing prostate cancer surgery. This progress is an important milestone as we work toward making erectile function rehabilitation a realistic expectation rather than an exception.”
In total, the prospective pilot study included 10 men who were potent before undergoing RARP. All patients received the CaverSTIM implant during the procedure and were asked to activate the device every day during the 6 months of follow-up.4
Overall, use of the device was shown to be safe and feasible, with no device explantations, device-relation infections, nor pain reported during stimulation. Two patients reported mild, transient discomfort. Implantation of the device added approximately 45 minutes to the RARP procedure.
Patients in the study also showed promising early functional outcomes, with 9 of 10 patients regaining potency following prostatectomy. Many patients in the trial were also able to resume unaided sexual intercourse.
Based on these results, Comphya announced plans to initiate a larger controlled clinical trial of the CaverSTIM device following completion of the pilot studies. The larger scale trial would build on these initial studies by further assessing the safety, tolerability, and efficacy of the device in restoring erectile function post-prostatectomy. The company also noted that use of the CaverSTIM device is being explored for other neurogenic causes of erectile dysfunction, such as spinal cord injury.
Investigators also published a scientific review outlining the rationale for implantable neurostimulation for managing post-prostatectomy erectile dysfunction. According to the authors, this approach is backed by 150 years of research showing erection responses following electrical stimulation.
Electrical neurostimulation of the penis, they explain, targets the penile-nerve supply that may be impaired by disease, injury, or aging, thus promoting authentic nerve functioning. The authors argue that this approach may address limitations of existing treatments by acting as a restorative therapy rather than a compensatory one.

Rodrigo Fraga, PhD
“The strength of this technology lies in its alignment with our understanding of erectile neurophysiology,” concluded co-author Rodrigo Fraga, PhD, COO of Comphya, in the news release. “We are grateful to Dr. [Arthur] Burnett, and the other co-authors for advancing this work, which we believe will represent a cornerstone for the field of neurostimulation and erectile dysfunction management. By stimulating the cavernous nerves at a time when injury is predictable, we may be able to promote neural rehabilitation and facilitate functional recovery rather than accepting postoperative erectile dysfunction as inevitable. While larger controlled trials are required, the early data strongly support continued clinical investigation.”
* “We are grateful to Dr. [Arthur] Burnett, and the other co-authors for advancing this work, which we believe will represent a cornerstone for the field of neurostimulation and erectile dysfunction management. By stimulating the cavernous nerves at a time when injury is predictable, we may be able to promote neural rehabilitation and facilitate functional recovery rather than accepting postoperative erectile dysfunction as inevitable. While larger controlled trials are required, the early data strongly support continued clinical investigation.”
Key Takeaways
- The CaverSTIM device demonstrated safety and feasibility in a first-in-man study, with 9 out of 10 patients regaining potency post-RARP.
- The study reported no device-related infections or pain, and only mild, transient discomfort in two patients.
- A larger clinical trial is planned to further evaluate the device's safety, tolerability, and efficacy in restoring erectile function.
- Neurostimulation targets impaired penile-nerve supply, potentially offering a restorative therapy for erectile dysfunction rather than a compensatory one.

CaverSTIM device shows initial promise for post-prostatectomy erectile dysfunction | Urology Times
The results highlight the early clinical potential of the device for restoring erectile function post-prostatectomy.
Data from a first-in-man clinical study (NCT05650866) of the CaverSTIM device have been published in BJU International, showing encouraging outcomes with the implantable cavernous nerve neurostimulator in restoring erectile function following robot-assisted radical prostatectomy (RARP).1
In addition to the early phase trial results, a review on the scientific rationale for using implantable neurostimulation was concurrently published in Nature Urology Review.2

Pim van Wesel
“These publications reflect a major step forward for CaverSTIM and for Comphya,” said Pim van Wesel, CEO of Comphya, in a news release from the company.2 “Seeing our technology validated in a first-in-man clinical study reinforces our confidence that neuromodulation can meaningfully improve quality-of-life outcomes for men undergoing prostate cancer surgery. This progress is an important milestone as we work toward making erectile function rehabilitation a realistic expectation rather than an exception.”
First-in-man studyIn total, the prospective pilot study included 10 men who were potent before undergoing RARP. All patients received the CaverSTIM implant during the procedure and were asked to activate the device every day during the 6 months of follow-up.4
Overall, use of the device was shown to be safe and feasible, with no device explantations, device-relation infections, nor pain reported during stimulation. Two patients reported mild, transient discomfort. Implantation of the device added approximately 45 minutes to the RARP procedure.
Patients in the study also showed promising early functional outcomes, with 9 of 10 patients regaining potency following prostatectomy. Many patients in the trial were also able to resume unaided sexual intercourse.
Based on these results, Comphya announced plans to initiate a larger controlled clinical trial of the CaverSTIM device following completion of the pilot studies. The larger scale trial would build on these initial studies by further assessing the safety, tolerability, and efficacy of the device in restoring erectile function post-prostatectomy. The company also noted that use of the CaverSTIM device is being explored for other neurogenic causes of erectile dysfunction, such as spinal cord injury.
Rationale for neurostimulationInvestigators also published a scientific review outlining the rationale for implantable neurostimulation for managing post-prostatectomy erectile dysfunction. According to the authors, this approach is backed by 150 years of research showing erection responses following electrical stimulation.
Electrical neurostimulation of the penis, they explain, targets the penile-nerve supply that may be impaired by disease, injury, or aging, thus promoting authentic nerve functioning. The authors argue that this approach may address limitations of existing treatments by acting as a restorative therapy rather than a compensatory one.

Rodrigo Fraga, PhD
“The strength of this technology lies in its alignment with our understanding of erectile neurophysiology,” concluded co-author Rodrigo Fraga, PhD, COO of Comphya, in the news release. “We are grateful to Dr. [Arthur] Burnett, and the other co-authors for advancing this work, which we believe will represent a cornerstone for the field of neurostimulation and erectile dysfunction management. By stimulating the cavernous nerves at a time when injury is predictable, we may be able to promote neural rehabilitation and facilitate functional recovery rather than accepting postoperative erectile dysfunction as inevitable. While larger controlled trials are required, the early data strongly support continued clinical investigation.”
Last edited by a moderator: