Nelson Vergel
Founder, ExcelMale.com
What Every Man Should Know About Prostatitis
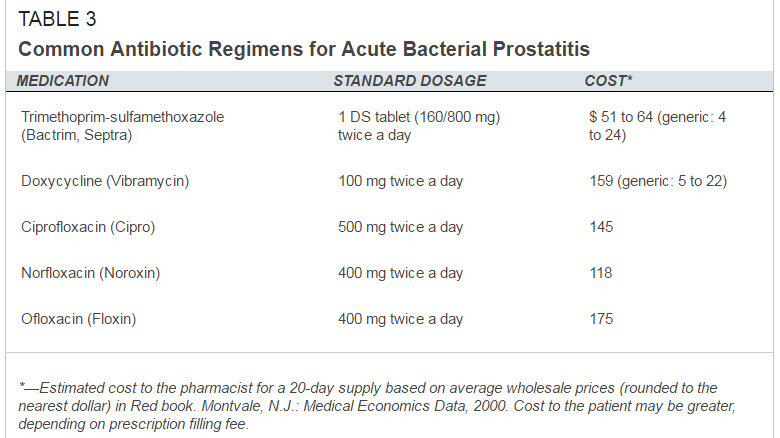
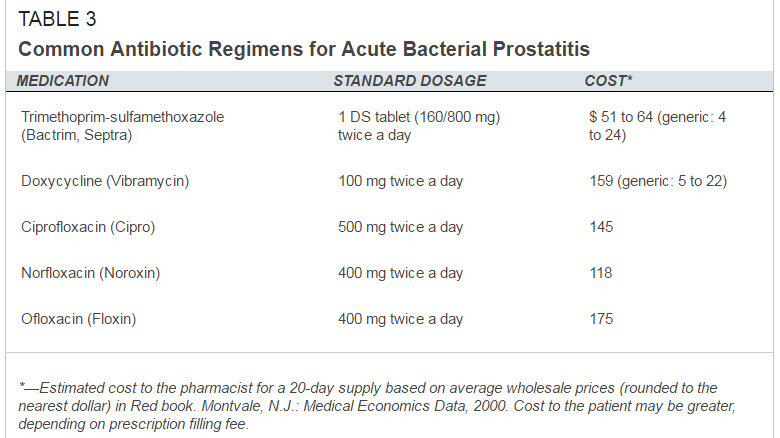
The term prostatitis is applied to a series of disorders, ranging from acute bacterial infection to chronic pain syndromes, in which the prostate gland is inflamed. Patients present with a variety of symptoms, including urinary obstruction, fever, myalgias, decreased libido or impotence, painful ejaculation and low-back and perineal pain. Physical examination often fails to clarify the cause of the pain. Cultures and microscopic examination of urine and prostatic secretions before and after prostatic massage may help differentiate prostatitis caused by infection from prostatitis with other causes. Because the rate of occult infection is high, a therapeutic trial of antibiotics is often in order even when patients do not appear to have bacterial prostatitis. If the patient responds to therapy, antibiotics are continued for at least three to four weeks, although some men require treatment for several months. A patient who does not respond might be evaluated for chronic nonbacterial prostatitis, in which nonsteroidal anti-inflammatory drugs, alpha-blocking agents, anticholinergic agents or other therapies may provide symptomatic relief. (Ref )
I discovered I had a bad case of prostatitis last month. I had back ache, pain under my belly button, tender perineum and a bloated feeling. I thought my IBS was acting out but my doctor told me prostatitis related referred pain is common. My urine came back normal but I was put on Cipro for 11 days. At the second day, my symptoms disappeared.
My symptoms just returned after a month. I may have refractory prostatitis, so starting a second cycle now using doxycycline.
In my research to try to find out more information about chronic prostatitis, I found out more than 90 percent of men with prostatitis meet the criteria for chronic nonbacterial prostatitis/chronic pelvic pain syndrome (CNP/CPPS).
Like many such poorly understood conditions, CNP/CPPS remains a challenging syndrome. Patients usually have symptoms consistent with prostatitis, such as painful ejaculation or pain in the penis, testicles or scrotum. They may complain of low back pain, rectal or perineal pain, or even pain along the inner aspects of the thighs. They often have irritative or obstructive urinary symptoms and decreased libido or impotence. As a rule, these patients do not have recurrent urinary tract infections. The physical examination is usually unremarkable, but patients may have a tender prostate. (Ref )
Asymptomatic Prostatitis
Information presented at the NIH consensus conference added asymptomatic prostatitis as a new category, partly because of the widespread use of the prostate-specific antigen (PSA) test.
Clearly, symptomatic bacterial prostatitis can elevate the PSA test to abnormal levels. Asymptomatic prostatitis may also elevate the PSA level. In addition, patients who are being evaluated for other prostatic disease may be found on biopsy to have prostatitis. There are no studies elucidating the natural history or appropriate therapy of this condition. It does appear that PSA levels return to normal four to six weeks after a 14-day course of antibiotics. Treatment is routinely recommended only in patients with chronic asymptomatic prostatitis known to elevate the PSA level. In these patients, it may be prudent to treat before drawing subsequent PSA samples.
The post What Every Man Should Know About Prostatitis appeared first on Testosterone Wisdom.
Continue reading...
The term prostatitis is applied to a series of disorders, ranging from acute bacterial infection to chronic pain syndromes, in which the prostate gland is inflamed. Patients present with a variety of symptoms, including urinary obstruction, fever, myalgias, decreased libido or impotence, painful ejaculation and low-back and perineal pain. Physical examination often fails to clarify the cause of the pain. Cultures and microscopic examination of urine and prostatic secretions before and after prostatic massage may help differentiate prostatitis caused by infection from prostatitis with other causes. Because the rate of occult infection is high, a therapeutic trial of antibiotics is often in order even when patients do not appear to have bacterial prostatitis. If the patient responds to therapy, antibiotics are continued for at least three to four weeks, although some men require treatment for several months. A patient who does not respond might be evaluated for chronic nonbacterial prostatitis, in which nonsteroidal anti-inflammatory drugs, alpha-blocking agents, anticholinergic agents or other therapies may provide symptomatic relief. (Ref )
I discovered I had a bad case of prostatitis last month. I had back ache, pain under my belly button, tender perineum and a bloated feeling. I thought my IBS was acting out but my doctor told me prostatitis related referred pain is common. My urine came back normal but I was put on Cipro for 11 days. At the second day, my symptoms disappeared.
My symptoms just returned after a month. I may have refractory prostatitis, so starting a second cycle now using doxycycline.
In my research to try to find out more information about chronic prostatitis, I found out more than 90 percent of men with prostatitis meet the criteria for chronic nonbacterial prostatitis/chronic pelvic pain syndrome (CNP/CPPS).
Like many such poorly understood conditions, CNP/CPPS remains a challenging syndrome. Patients usually have symptoms consistent with prostatitis, such as painful ejaculation or pain in the penis, testicles or scrotum. They may complain of low back pain, rectal or perineal pain, or even pain along the inner aspects of the thighs. They often have irritative or obstructive urinary symptoms and decreased libido or impotence. As a rule, these patients do not have recurrent urinary tract infections. The physical examination is usually unremarkable, but patients may have a tender prostate. (Ref )
Asymptomatic Prostatitis
Information presented at the NIH consensus conference added asymptomatic prostatitis as a new category, partly because of the widespread use of the prostate-specific antigen (PSA) test.
Clearly, symptomatic bacterial prostatitis can elevate the PSA test to abnormal levels. Asymptomatic prostatitis may also elevate the PSA level. In addition, patients who are being evaluated for other prostatic disease may be found on biopsy to have prostatitis. There are no studies elucidating the natural history or appropriate therapy of this condition. It does appear that PSA levels return to normal four to six weeks after a 14-day course of antibiotics. Treatment is routinely recommended only in patients with chronic asymptomatic prostatitis known to elevate the PSA level. In these patients, it may be prudent to treat before drawing subsequent PSA samples.
The post What Every Man Should Know About Prostatitis appeared first on Testosterone Wisdom.
Continue reading...
















