Nelson Vergel
Founder, ExcelMale.com
Rastrelli G, Cipriani S, Lotti F, et al. 186 - Testosterone replacement
therapy is able to reduce prostate inflammation in men with BPH, metabolic
syndrome and hypogonadism: Preliminary results from a randomized placebo
controlled clinical trial. European Urology Supplements 2018;17:e269.
Testosterone replacement therapy is able to reduce prostate inflammation in men with BPH, metabolic syndrome and hypogonadism: Preliminary results from a randomized placebocontrolled clinical trial
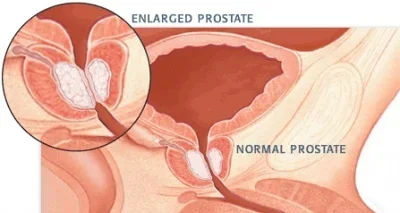
Introduction & Objectives: BPH results from prostate tissue inflammation,
which frequently occurs in men with metabolic syndrome (MetS). MetS is often
associated with low testosterone (T). Recent evidence shows that low, rather
than high, T levels are associated with BPH/lower urinary tract symptoms
(LUTS).
The aim of the study was to evaluate if T replacement therapy (TRT) for 6
months in BPH men with MetS and low T, is able to improve LUTS and prostate
inflammation (as assessed by ultrasound and gene expression in prostate
tissue).
Materials & Methods: Ethical Committee approval has been obtained for the
trial. 120 men in the waiting list for BPH surgery and diagnosed with MetS
were enrolled in the clinical trial. Informed consent was obtained from each
patient. According to total T (TT) and calculated free T (cFT), they were
categorized into eugonadal (TT?12 nmol/L and cFT?225 pmol/L; n=48) and
hypogonadal men (TT<12 nmol/L and/or cFT<225 pmol/L; n=72).
Hypogonadal men were randomly assigned to receive T gel 2% (5 g/daily) or
placebo for 6 months. At baseline and follow-up visit (after 6 months), all
men filled out the International Prostatic Symptoms Score (IPSS) and
NIH-Chronic Prostatitis Symptom Index (NIH-CSPI) questionnaires and
underwent a trans-rectal prostate ultrasound. After surgery, prostate tissue
was collected.
Results: After adjusting for the baseline value, together with age, TT and
waist circumference, NIH-CSPI total score significantly decreased in both
the groups (p<0.001 vs. baseline), whereas IPSS total score did not change
in any of the groups. IPSS bother score significantly decreased only in
T-treated (p=0.042 vs. baseline value).
Although a significant increase in total prostate and adenoma volume
occurred in T-treated (both p<0.05 vs. the baseline value), T arm was
characterised by a significant decrease in ultrasound markers of prostate
inflammation, including arterial velocity and acceleration (both p<0.01 vs.
baseline value).
In a subset of patients (9 eugonadal, 11 placebo and 9 T-treated), the
expression by prostate tissue of inflammatory markers was evaluated. COX2,
MCP1 and RORC were found significantly decreased in T-treated as compared
with the placebo arm (all p<0.01) and for COX2 and MCP1 even in comparison
with eugonadal men (both p<0.05).
Conclusions: Six-month treatment with T gel 2% in hypogonadal men with BPH
and MetS is able to improve several clinical, ultrasound and molecular
proxies of prostate inflammation.














