Last edited by a moderator:
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
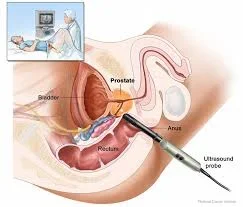
Is DHT the Cause of BPH ( Prostate Enlargement ) or is it Estradiol?
- Thread starter lexer
- Start date
Vince Carter
Banned
Finasteride preserves your prostate by chemically neutering you. Read up on Post Finasteride Syndrome.
BPH and prostate cancer are not the same thing. On the latter I believe the verdict is still out. That was my conclusion after reading up. Estrogen role is very poorly understood, and it's not just all estrogen. In some cases estrogen helps to grow tumors, but in others it is protective from further growth.
My understanding of DHT is that the prostate has a threshold for how much it's going to process. Beyond that and within physiological levels it makes no difference.
I'm not in the medical field though. I could be misinterpreting some things. I read a number of articles, including this one:
Testosterone Replacement and Prostate Cancer - Life Extension
My understanding of DHT is that the prostate has a threshold for how much it's going to process. Beyond that and within physiological levels it makes no difference.
I'm not in the medical field though. I could be misinterpreting some things. I read a number of articles, including this one:
Testosterone Replacement and Prostate Cancer - Life Extension
Rapamycin decreases chemically-induced benign prostate hyperplasia in rats
LINK TO FULL ARTICLE:
Rapatar, a nanoformulation of rapamycin, decreases chemically-induced benign prostate hyperplasia in rats
LINK TO FULL ARTICLE:
Rapatar, a nanoformulation of rapamycin, decreases chemically-induced benign prostate hyperplasia in rats
...we showed that, in a dose-dependent manner,
Rapatar (a new oral formulation of rapamycin) prevented
sulpiride-induced BPH. Sulpiride induced cystic enlarged
acini, with atrophic and degenerative changes, loss of
secretion and destruction of the epithelial lining. In this
model, Rapatar normalized both the weight of prostate
lobes and their tissue architecture. Rapatar decreased the
cystic transformation of acini caused by sulpiride. Most
of the acini were lined with secretory epithelium. In the
surrounding area, a fewer number of small acini were
observed. Thus, Rapatar abrogated prostate enlargement.
Rapatar also prevented pathological histological
alterations caused by testosterone, while minimally
affecting the lobes weight.
madman
Super Moderator
I understand how finasteride works. What i am asking is why so many people say estrogen is the cause of BPh and not DHT when obviously finasteride lowers dht and the prostate shrinks???
Androgens and estrogens in benign prostatic hyperplasia: past, present and future
Nelson Vergel
Founder, ExcelMale.com
Excellent question!
Here is the best DHT review paper out there.
Some quotes
"Circulating levels of DHT in response to testosterone replacement therapy (TRT) do not correlate with those found in androgen sensitive tissue (e.g., prostate, adipose, muscle) due to local regulatory mechanisms that tightly control intracellular androgen homeostasis."
"The clinical benefits associated with lowered serum DHT levels after 5AR-Is appear to have led to the misconception that circulating DHT is an important stimulus for androgenic action in the prostate gland. However, studies in which serum DHT concentrations were markedly elevated by exogenous administration of DHT had almost no effect on prostate DHT concentrations, prostate size, and lower urinary tract symptoms (see “Intraprostatic Control Of DHT in the Presence of Fluctuating Levels of Circulating Androgens” and associated references). The reason for this highlights fundamentally important control mechanisms in androgen target tissues that finely regulate pathways for androgen synthesis and degradation to maintain DHT homeostasis. These intracellular processes do not appear to be affected by circulating DHT concentrations. Furthermore, it is well documented that DHT can be synthesized in androgen-sensitive tissues such as prostate from substrates other than T (e.g., from 17-hydroxypregnenolone and 17-hydroxyprogesterone in what is termed the “backdoor” pathway and from 5α-androstane-3α, 17-β-diol via the intracrine reverse synthesis pathway) (4). We will also explore the implications of modest increases in serum DHT that are seen with T replacement therapy (TRT; including, for completeness, DHT preparations) for male hypogonadism and discuss why these likely have minimal clinical implications for men treated with androgens."
Source
Here is the best DHT review paper out there.
Some quotes
"Circulating levels of DHT in response to testosterone replacement therapy (TRT) do not correlate with those found in androgen sensitive tissue (e.g., prostate, adipose, muscle) due to local regulatory mechanisms that tightly control intracellular androgen homeostasis."
"The clinical benefits associated with lowered serum DHT levels after 5AR-Is appear to have led to the misconception that circulating DHT is an important stimulus for androgenic action in the prostate gland. However, studies in which serum DHT concentrations were markedly elevated by exogenous administration of DHT had almost no effect on prostate DHT concentrations, prostate size, and lower urinary tract symptoms (see “Intraprostatic Control Of DHT in the Presence of Fluctuating Levels of Circulating Androgens” and associated references). The reason for this highlights fundamentally important control mechanisms in androgen target tissues that finely regulate pathways for androgen synthesis and degradation to maintain DHT homeostasis. These intracellular processes do not appear to be affected by circulating DHT concentrations. Furthermore, it is well documented that DHT can be synthesized in androgen-sensitive tissues such as prostate from substrates other than T (e.g., from 17-hydroxypregnenolone and 17-hydroxyprogesterone in what is termed the “backdoor” pathway and from 5α-androstane-3α, 17-β-diol via the intracrine reverse synthesis pathway) (4). We will also explore the implications of modest increases in serum DHT that are seen with T replacement therapy (TRT; including, for completeness, DHT preparations) for male hypogonadism and discuss why these likely have minimal clinical implications for men treated with androgens."
Source
Nelson Vergel
Founder, ExcelMale.com
Differentiation. 2011 Nov-Dec;82(4-5):184-99. doi: 10.1016/j.diff.2011.04.006. Epub 2011 May 26.
Androgens and estrogens in benign prostatic hyperplasia: past, present and future.
Nicholson TM1, Ricke WA.
Abstract
Benign prostatic hyperplasia (BPH) and associated lower urinary tract symptoms (LUTS) are common clinical problems in urology. While the precise molecular etiology remains unclear, sex steroids have been implicated in the development and maintenance of BPH. Sufficient data exists linking androgens and androgen receptor pathways to BPH and use of androgen reducing compounds, such as 5α-reductase inhibitors which block the conversion of testosterone into dihydrotestosterone, are a component of the standard of care for men with LUTS attributed to an enlarged prostate. However, BPH is a multifactorial disease and not all men respond well to currently available treatments, suggesting factors other than androgens are involved. Testosterone, the primary circulating androgen in men, can also be metabolized via CYP19/aromatase into the potent estrogen, estradiol-17β. The prostate is an estrogen target tissue and estrogens directly and indirectly affect growth and differentiation of prostate. The precise role of endogenous and exogenous estrogens in directly affecting prostate growth and differentiation in the context of BPH is an understudied area. Estrogens and selective estrogen receptor modulators (SERMs) have been shown to promote or inhibit prostate proliferation signifying potential roles in BPH. Recent research has demonstrated that estrogen receptor signaling pathways may be important in the development and maintenance of BPH and LUTS; however, new models are needed to genetically dissect estrogen regulated molecular mechanisms involved in BPH. More work is needed to identify estrogens and associated signaling pathways in BPH in order to target BPH with dietary and therapeutic SERMs.
Androgens and estrogens in benign prostatic hyperplasia: past, present and future.
Nicholson TM1, Ricke WA.
Abstract
Benign prostatic hyperplasia (BPH) and associated lower urinary tract symptoms (LUTS) are common clinical problems in urology. While the precise molecular etiology remains unclear, sex steroids have been implicated in the development and maintenance of BPH. Sufficient data exists linking androgens and androgen receptor pathways to BPH and use of androgen reducing compounds, such as 5α-reductase inhibitors which block the conversion of testosterone into dihydrotestosterone, are a component of the standard of care for men with LUTS attributed to an enlarged prostate. However, BPH is a multifactorial disease and not all men respond well to currently available treatments, suggesting factors other than androgens are involved. Testosterone, the primary circulating androgen in men, can also be metabolized via CYP19/aromatase into the potent estrogen, estradiol-17β. The prostate is an estrogen target tissue and estrogens directly and indirectly affect growth and differentiation of prostate. The precise role of endogenous and exogenous estrogens in directly affecting prostate growth and differentiation in the context of BPH is an understudied area. Estrogens and selective estrogen receptor modulators (SERMs) have been shown to promote or inhibit prostate proliferation signifying potential roles in BPH. Recent research has demonstrated that estrogen receptor signaling pathways may be important in the development and maintenance of BPH and LUTS; however, new models are needed to genetically dissect estrogen regulated molecular mechanisms involved in BPH. More work is needed to identify estrogens and associated signaling pathways in BPH in order to target BPH with dietary and therapeutic SERMs.
Last edited:
Nelson Vergel
Founder, ExcelMale.com
Serum Steroid and Sex Hormone-Binding Globulin Concentrations and the Risk of Incident Benign Prostatic Hyperplasia: Results From the Prostate Cancer Prevention Trial
Alan R. Kristal Jeannette M. Schenk YoonJu Song Kathryn B. Arnold Marian L. Neuhouser Phyllis J. Goodman Daniel W. Lin Frank Z. Stanczyk Ian M. Thompson
American Journal of Epidemiology, Volume 168, Issue 12, 15 December 2008, Pages 1416–1424.
Abstract
The authors conducted a nested case-control study of serum steroid concentrations and risk of benign prostatic hyperplasia (BPH), using data from the placebo arm of the Prostate Cancer Prevention Trial (1993–2003). Incident BPH over 7 years (n = 708) was defined as receipt of treatment, a report of 2 International Prostate Symptom Score (IPSS) values greater than 14, or 2 increases of 5 or more from baseline IPSS values with at least 1 value greater than or equal to 12. Controls (n = 709) were selected from men who reported no BPH treatment or any IPSS greater than 7. Baseline serum was analyzed for testosterone, estradiol, estrone, 5α-androstane-3α, 17β-diol-glucuronide, and sex hormone-binding globulin. Covariate-adjusted odds ratios contrasting the highest quartiles with the lowest quartiles of testosterone, estradiol, and testosterone:17β-diol-glucuronide ratio were 0.64 (95% confidence interval (CI): 0.43, 0.95; Ptrend = 0.04), 0.72 (95% CI: 0.53, 0.98; Ptrend = 0.09), and 0.64 (95% CI: 0.46, 0.89; Ptrend = 0.004), respectively. Findings did not differ by age, body mass index, time to BPH endpoint, or type of BPH endpoint. High testosterone levels, estradiol levels, and testosterone:17β-diol-glucuronide ratio are associated with reduced BPH risk, which may reflect decreased activity of 5-α-reductase. Genetic or environmental factors that affect the activity of 5-α-reductase may be important in the development of symptomatic BPH.
"Whether or not there is a relation of estrogens with BPH risk remains uncertain. Gann et al. (35) reported a positive association between estradiol and incident BPH surgery but only among men with low testosterone and only after controlling for estrone, which suggests that the strong collinearity of estrone and estradiol may have yielded an unstable statistical model. Rohrmann et al. (29) reported a positive association of estradiol with lower urinary tract symptoms. In contrast, both we and others (26, 27) found that estradiol was significantly and negatively associated with BPH. The prostate expresses both estrogen receptor β (in epithelium, where it inhibits growth) and estrogen receptor α (in stroma, where it promotes growth). There is little evidence that estrogen receptor α has a role in BPH (47), and thus a growth-inhibitory effect of estradiol could be consistent with reduced BPH risk. It is also possible that a high estradiol level simply reflects a high testosterone level, because estradiol in older men is almost exclusively formed by aromatization of testosterone. This picture is further complicated by observations in the Prostate Cancer Prevention Trial (48) and other studies (49–51) that abdominal obesity is a risk factor for BPH, because abdominal obesity also increases estradiol levels. Additional studies of the effects of estradiol on BPH pathogenesis are needed."
Full paper
Alan R. Kristal Jeannette M. Schenk YoonJu Song Kathryn B. Arnold Marian L. Neuhouser Phyllis J. Goodman Daniel W. Lin Frank Z. Stanczyk Ian M. Thompson
American Journal of Epidemiology, Volume 168, Issue 12, 15 December 2008, Pages 1416–1424.
Abstract
The authors conducted a nested case-control study of serum steroid concentrations and risk of benign prostatic hyperplasia (BPH), using data from the placebo arm of the Prostate Cancer Prevention Trial (1993–2003). Incident BPH over 7 years (n = 708) was defined as receipt of treatment, a report of 2 International Prostate Symptom Score (IPSS) values greater than 14, or 2 increases of 5 or more from baseline IPSS values with at least 1 value greater than or equal to 12. Controls (n = 709) were selected from men who reported no BPH treatment or any IPSS greater than 7. Baseline serum was analyzed for testosterone, estradiol, estrone, 5α-androstane-3α, 17β-diol-glucuronide, and sex hormone-binding globulin. Covariate-adjusted odds ratios contrasting the highest quartiles with the lowest quartiles of testosterone, estradiol, and testosterone:17β-diol-glucuronide ratio were 0.64 (95% confidence interval (CI): 0.43, 0.95; Ptrend = 0.04), 0.72 (95% CI: 0.53, 0.98; Ptrend = 0.09), and 0.64 (95% CI: 0.46, 0.89; Ptrend = 0.004), respectively. Findings did not differ by age, body mass index, time to BPH endpoint, or type of BPH endpoint. High testosterone levels, estradiol levels, and testosterone:17β-diol-glucuronide ratio are associated with reduced BPH risk, which may reflect decreased activity of 5-α-reductase. Genetic or environmental factors that affect the activity of 5-α-reductase may be important in the development of symptomatic BPH.
"Whether or not there is a relation of estrogens with BPH risk remains uncertain. Gann et al. (35) reported a positive association between estradiol and incident BPH surgery but only among men with low testosterone and only after controlling for estrone, which suggests that the strong collinearity of estrone and estradiol may have yielded an unstable statistical model. Rohrmann et al. (29) reported a positive association of estradiol with lower urinary tract symptoms. In contrast, both we and others (26, 27) found that estradiol was significantly and negatively associated with BPH. The prostate expresses both estrogen receptor β (in epithelium, where it inhibits growth) and estrogen receptor α (in stroma, where it promotes growth). There is little evidence that estrogen receptor α has a role in BPH (47), and thus a growth-inhibitory effect of estradiol could be consistent with reduced BPH risk. It is also possible that a high estradiol level simply reflects a high testosterone level, because estradiol in older men is almost exclusively formed by aromatization of testosterone. This picture is further complicated by observations in the Prostate Cancer Prevention Trial (48) and other studies (49–51) that abdominal obesity is a risk factor for BPH, because abdominal obesity also increases estradiol levels. Additional studies of the effects of estradiol on BPH pathogenesis are needed."
Full paper
Nelson Vergel
Founder, ExcelMale.com
Conclusion from above papers: Not as clear as it seems!
Just wanted to drop this here. My estrogen was between 15 and 20 non sensitive all my life. Yet my psa is 1.4 . I am 38yo, 1.4 is not really low for my age.I have seen many older relatives with psa of 0.5 range. I know at least 4 with such values.
I don’t know if it relative but I have for varicocele fixed at younger age, I still have very mild one and been told no need to fix that. But I may fix it anyway.
I don’t know if it relative but I have for varicocele fixed at younger age, I still have very mild one and been told no need to fix that. But I may fix it anyway.
Last edited:
DragonBits
Well-Known Member
Just wanted to drop this here. My estrogen was between 15 and 20 non sensitive all my life. Yet my psa is 1.4 m. I am 38yo, 1.4 is not really low for my age.I have seen many older relatives with psa of 0.5 range. I know at least 4 with such values.
I don’t know if it relative but I have for varicocele fixed at younger age, I still have very mild one and been told no need to fix that. But I may fix it anyway.
On a similar note, at age 43 my PSA was 2.1, and stayed in the range of 2.1-2.7 for the next 22 years, even with 5 years of TRT at age 57. My T has been both low and high during that time, likely E2 was fairly low and well as DHT likely being on the low side, even during most of the TRT. During the first 5 years of TRT (nebido) I kept measuring PSA but never measured Estradiol nor DHT.
But going on recent years, likely my E2 was fairly low as it is seldom high unless my total T gets above 1500. Even at total T of 2000 my E2 was 56, while high, isn't as high as one might expect for the total t. Outside of that one measurement of E2 at 56, the highest my E2 has been is 27 with all levels of total T.
At age 66 my PSA did up range to 3.2-4.8, no idea why, very unlikely cancer as I had several tests that indicate little likely hood of cancer. The move up was very likely triggered by resuming TRT at age 65, same TRT protocol as before (Nebido) though I did add HCG / DHEA, no idea if that was the reason for the jump up as stopping both of those (HCG/DHEA) didn't cause any lowering of the range.
I could theorize that HCG enabled an enlargement of the prostate, once larger it didn't shrink just because I stopped HCG, but really, the evidence is not strong enough to say for sure why PSA rose, it's as though it increased to what is more typical for my age of 67. I restated DHEA with no change in the PSA range that I mentioned.
DorianGray
Active Member
That's interesting @DragonBits. I wasn't aware HCG might have an effect. I'll be doing labs in a few weeks and will be curious to see if HCG I've been on has impacted PSA. It's been at .3-.4 for many decades now.
DragonBits
Well-Known Member
That's interesting @DragonBits. I wasn't aware HCG might have an effect. I'll be doing labs in a few weeks and will be curious to see if HCG I've been on has impacted PSA. It's been at .3-.4 for many decades now.
I don't know that HCG did have an effect. It's certainly in a related region and changing testicular levels of Testosterone / DHT / estrogen is more likely to have an effect Vs serum levels.
I saw one study where HCG was implicated in prostate growth, but it wasn't very convincing.
Much earlier I took clomid, which had no effect on PSA, raised my E2 / Testosterone but not enough to reduce symptoms of low T.
Although not for a long time, when I started trt last year,I did hcg maybe for 1 month followed by trt +hcg maybe for 6 month.I don't know that HCG did have an effect. It's certainly in a related region and changing testicular levels of Testosterone / DHT / estrogen is more likely to have an effect Vs serum levels.
I saw one study where HCG was implicated in prostate growth, but it wasn't very convincing.
Much earlier I took clomid, which had no effect on PSA, raised my E2 / Testosterone but not enough to reduce symptoms of low T.
Then I stopped everything for some time maybe two month. Retested psa and it went back to normal figure ! 1.4
also during Trt it went up by 0.3.before going back to normal level. this 0.3 figure was mentioned exactly in a published paper on the affect of trt on psa.
hCG Mixing Calculator
HCG Mixing Protocol Calculator
Similar threads
- Replies
- 0
- Views
- 163
- Replies
- 14
- Views
- 3K
- Replies
- 0
- Views
- 1K
- Replies
- 2
- Views
- 1K
Online statistics
- Members online
- 4
- Guests online
- 1,013
- Total visitors
- 1,017
Totals may include hidden visitors.
Latest posts
-
-
-
-
-
-
-
Advice on where to find trustworthy peptides
- Latest: Nelson Vergel
-