madman
Super Moderator
Priapism or Prolonged Erection: Is 4 – 6 Hours of Cavernous Ischemia the Time Point of Irreversible Tissue Injury?
AbstractIntroduction. Ischemic priapism remains a significant cause of morbidity among men. To date, the precise time when penile ischemia results in perma
Priapism or Prolonged Erection: Is 4−6 Hours of Cavernous Ischemia the Time Point of Irreversible Tissue Injury? (2022)
Snir Dekalo, MD, Noah Stern, MD, Gregory A. Broderick, MD, and Gerald Brock, MD, FRCPC
ABSTRACT
Introduction
Ischemic priapism remains a significant cause of morbidity among men. To date, the precise time when penile ischemia results in permanent, non-reversible cavernosal smooth muscle injury, compromising subsequent erectile integrity, remains ill-defined.
Objectives
To review the medical literature pertaining to ischemic priapism, focusing on factors that predict the exact timeline of irreversible cavernous tissue injury.
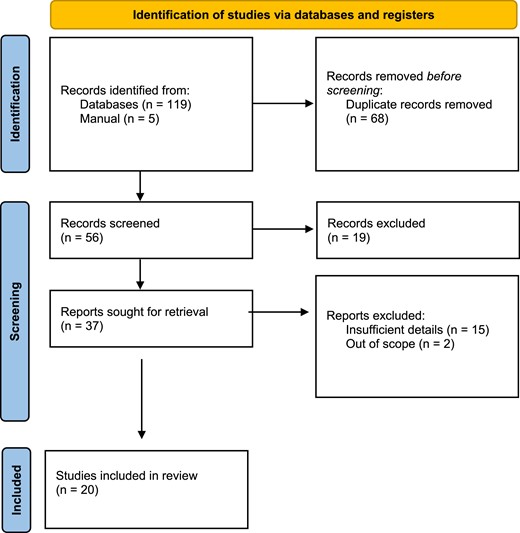
Methods
A comprehensive literature search was performed. Our search included both publications on animal models and retrospective clinical series through January 2022. Articles were eligible for inclusion if they contained original data regarding nonreversible tissue injury on histology and/or provided a timeline of erectile function loss or preservation and had full text available in English.
Results
Innovative studies in the 1990s using in-vitro models with strips of rabbit, rat, canine, and monkey corpus cavernosal tissue demonstrated that anoxia eliminated spontaneous contractile activity and reduced tissue responsiveness to electrical field stimulation or pharmacological agents. The same models demonstrated that the inhibitory effects of field-stimulated relaxation were mediated by nitric oxide. Subsequent studies using similar models demonstrated that exposure of corpus cavernosum smooth muscle to an acidotic environment impairs its ability to contract. A pH of 6.9 was chosen for these experiments based on a case series of men with priapism, in whom a mean pH of 6.9 was measured in corporal blood after 4−6 hours of priapism. Invivo animal studies demonstrated that after erection periods of 6−8 hours, microscopy shows sporadic endothelial defects but otherwise normal cavernous smooth muscle. In these studies, greater durations of ischemic priapism were shown to result in more pronounced ultrastructural changes and presumably irreversibility. In studies involving human corporal tissues, samples were obtained from men who had experienced priapism for at least 12 hours. Overall, erectile function outcome data is deficient in priapism reporting, especially within treatment windows of less than 6 hours. Some reports on ischemic priapism have documented good erectile function outcomes with reversal by 12 hours.
Conclusion
Based on our extensive review of animal models and clinical reports, we found that many clinical papers rely on the same small set of animal studies to suggest the time point of irreversible ischemic damage at 4−6 hours. Our review suggests an equal number of retrospective clinical studies demonstrate that ischemic priapism reversed within 6−12 hours may preserve erectile function in many patients.
INTRODUCTION
Normal penile erection is only possible when a highly orchestrated series of physiologic events occur in a specific order. The essential components are adequate neurotransmitter-mediated cavernosal smooth muscle relaxation, which induces the local endothelial release of vasoactive substances. This then leads to enhanced dilation of the cavernosal arteries. This results in enhanced arterial inflow with corporal expansion and venous occlusion, culminating in a rigid erection. A deficiency in any of these components will compromise the quality, length, rigidity, and duration of the penile erection, resulting in loss of function.1
Priapism is classically characterized as either ischemic (venoocclusive), high flow (arterial), or intermittent (stuttering). Priapism describes an erection that continues more than 4 hours beyond sexual stimulation and orgasm or is unrelated to sexual stimulation. Ischemic priapism is a persistent erection marked by the rigidity of the corpora cavernosa with little or no cavernous arterial inflow. As a consequence of ischemia, the corporal environment deprived of oxygenation becomes hypercarbic and acidotic; the severity of these changes is time-dependent.2
Despite these facts, the critical importance of defining the precise timeline when penile ischemia results in permanent, irreversible cavernosal smooth muscle, and penile vascular injury, remains ill-defined even to this day. Clinical guidance is based largely on historical reports and most contemporary scholarly manuscripts cite secondary references that never even attempted to address the timeline of histological and cellular injury that penile ischemia is believed to cause.
Given this knowledge gap, there is a need for a careful methodological review of the English language medical literature pertaining to ischemic priapism focusing not on diagnostics, therapeutic, or surgical interventions, but rather on the particular inducing events and patient factors that may alter the timeline of nonreversible tissue injury.
The evaluation of the medical literature, searching for credible studies, and endpoints, and assessing tissue integrity, and erectile function loss or preservation has value to the clinician and patient alike. Knowing the specific time frame when a particular patient is likely to sustain a non-reversible ischemic end-organ injury is critical for clinical management and patient information.
The most recent American Urological Association (AUA) and Sexual Medicine Society of North America (SMSNA) Priapism Guidelines3 describe ischemic injury and necrosis beginning as early as 4−6 hours post onset of ischemic priapism. We chose to initiate this review to specifically examine the evidence supporting the guideline dictum: Although some forms of priapism are non-urgent in nature, prolonged (>4 hours) acute ischemic priapism, characterized by little or no cavernous blood flow and abnormal cavernous blood gases (ie, hypoxic, hypercarbic, acidotic) represents a medical emergency and may lead to cavernosal fibrosis and subsequent erectile dysfunction.
If we accept the hypothesis that 6 hours of ischemia leads to irreversible tissue damage, then there should be clear clinical evidence of detriment to erectile function. The 2021 AUA/SMSNA Guidelines cite two articles as evidence showing edema and atrophy as early as 6 hours, however, neither of these reports investigated patients with priapism less than 10 hours.4
*The purpose of this review is to critically appraise the available literature regarding histologic changes associated with ischemic priapism, in order to better understand and characterize the early pathologic and irreversible changes to penile structure and function.
Results
*In Vitro Animal Models
*In-Vivo Animal Models
*Human Models and Clinical Data
Discussion
There exist few urological emergencies that are more common or impactful on a patient’s quality of life than ischemic priapism. The epidemiologically reported incidence rate of 1.5 per million is likely underestimated as this data reflects only spontaneous priapism and omits medication-induced events, which would dramatically increase the numbers of men with priapism who need medical attention.25 In fact, it is the very rare urology trainee who does not become an expert at managing men with ischemic priapism. Whether priapism is from self-injection of a vasoactive agent among men with erectile dysfunction, in-office pharmaco-testing for vascular erectile integrity in Peyronie’s disease, or sickle cell disease or idiopathic ischemic priapism, the natural history of delayed or untreated ischemic events is loss of erectile potential.
Though significant efforts have refined our understanding of when recovery of erectile function may be irrecoverable over the past 40 years, the precise time point when ischemic priapism can be safely reversed remains unclear. Understanding the relationship between the duration of ischemia and the development of corporal fibrosis is essential for clinical guidelines and has medicolegal implications for counseling and the timing of interventions.
Excellent work19 has refined our understanding of when recovery of erectile function is unlikely post-ischemic priapism, with most reports suggesting 36−48 hours. What is not well-known is when the histological and subsequential functional changes begin. Critical to optimal management is an evidence-based understanding of the pathophysiology, the time course of the condition, and therapeutic options available to reverse or delay the tissue effects of ischemic priapism, prevent future episodes, and ensure erectile integrity.
For the clinician, the ability to inform the patient about an evidence-based timeline, expectations of outcomes, and clear direction for acute and chronic management are critical. Counseling men who perform penile self-injection for ED should be highlighted by a clear timeline to avoid irreversible tissue injury. Equally important, timeline counseling for intervention might spare treating physicians’ legal liability.
Contemporary medical literature has only weak evidence to support a definitive timeline between prolonged erection, reversible priapism, and irreversible corporal pathology resulting from failed ischemic priapism at more than 36 hours. Obtaining human penile tissue in cases of short-duration ischemic priapism (typically defined in most studies as <12 hours) is difficult and obviously unethical as the majority of these patients are reversed with minimally invasive techniques. In cases where surgical management and obtaining a corporal sample is feasible, the typical time elapsed is beyond 36 hours. Sampling corporal tissues after 36 hours provides little insight into the nature of the physiologic process leading up to the time point.19,23,24
The challenges of predicting human physiologic responses based on animal model data are significant. The varieties of animal models include: 1) In vivo modeling with cats, mice, rats, and rabbits exposed to a variety of experimental parameters to induce ischemia through reducing inhaled tidal volumes, intracavernous injections, genetic engineering, and vacuum constriction devices 2) In vitro models relying on animal corporal tissue harvested and exposed to organ baths with altered environments: hypoxia, acidosis, and glucose content.26Animal corporal tissue is also used for cell culture and binding assays. To date, there is no single standardized experimental model to address the remaining physiologic questions surrounding the ischemic priapism timeline.
Among the variables which may alter the ischemia response of man compared to cat, mouse, rat, monkey, dog, or rabbit models are that the animals are typically young and healthy. The ischemia is usually rapidly induced and profound, without intermittency of blood flow. The metabolism of the animal is many folds more rapid than even healthy men,9 and other variables which may or may not be reported include: the hydration status of the animal model, glucose levels, stress levels, anesthetic agents, blood pressure, and the surgical prep used, each of which can be impactful. Additionally, no ischemic host response occurs in tissue cultures or organ baths. The experimental modeling may not represent what occurs in man.
Animal models have provided important insights into the tissue effects of ischemia. They have defined a relationship between ischemic priapism and the critical role of pH, contents of glucose, oxygen, and carbon dioxide to be critical in predicting cavernosal tissue injury.2,9 Time is undeniably a factor. Broderick et al established the role of acidosis, hypercarbia, and hypoxia in corporal smooth muscle physiology. The basic science investigations were inspired by a small clinical study of 14 patients with prolonged erections (105−342 minutes). Of interest, the clinical series was composed of 366 ‘new impotence patients’, 14 of whom developed prolonged erection following intracavernous pharmacotesting with Prostaglandin E1. Within that 6-hour time window, the authors documented statistically significant trends in penile blood gas aspirates toward deoxygenation, acidosis, and hypercarbia.1,27 Each of these patients went on to successfully use PGE1 at reduced home dosing. It is our belief that this small clinical series followed by many authors applying diverse animal modeling has focused attention on the 6-hour window. While the animal studies do substantiate the cascade of changes in corporal smooth muscle that follow penile compartment syndrome we define as ischemic priapism, they do not specify the tipping point of irreversibility. It is notable that in the human condition of sickle cell disease priapism reversal by aspiration/irrigation/phenylephrine up to 12 hours can be successful and result in spontaneous erectile responses for some patients and responsivity to PDE type 5 inhibitors in others.28
Individual peer-reviewed research and clinical guidelines composed by medical societies carry weight, are important documents, and are designed to provide a standard of care for groups of patients based on evidence. Recommendations are weighted for the level of supporting evidence. The natural history of ischemic priapism is days to weeks of penile pain and subsequent corporal fibrosis resulting in penile shortening and complete erectile dysfunction. The challenge for all priapism guidelines committees has been to draw an arbitrary line in the sand and say at this point intervention is warranted, has a high degree of success at achieving reversal, and should result in favorable erectile function outcomes if applied judiciously with the clinical and surgical steps recommended. As such, we the authors of this review do endorse interventions as outlined in the AUA/SMSNA Guidelines on priapism. Our review highlights the understanding of the physiologic sequelae of corporal ischemia. The literature supports the time-dependent nature of ischemic priapism but also supports the plasticity of corporal smooth muscle to recover with the reversal of ischemia. Unreversed ischemic priapism is a disaster for the patient and all efforts should be made to avoid it if possible and reverse it when encountered. The 4-6 hours timeline is the sounding of an alarm that should be heeded by clinicians.
CONCLUSIONS
Our review of the basic and clinical literature published over the past 40 years reveals an interesting insight into the world of research. Animal models provided the first understanding of how an ischemic environment could injure cavernosal smooth muscle and other critical tissues within the penis. A consensus has arrived at that pH, glucose, hypoxia, and time, were critical in determining the extent of the injury. Host factors such as the down-regulation of reactive oxygen species, and upregulation of protective pathways such as reactive oxygen scavenger formation along with other host defense mechanisms all play a role in defining the timing and extent of an individual patient’s penile tissue injury. The remaining challenge for guideline authors and medical societies however is to define a timeline that should be applied to a population at risk for penile ischemia, understanding the potential inter-individual variability, to mitigate risks of consequent erectile dysfunction.
The animal model studies have been complemented by innovative clinical reports, documenting the reversible nature of ischemic priapism if treated early by aspiration, irrigation, and alpha agonist injections. A prolonged erection can be reversed with the anticipation of a favorable outcome the earlier the reversal is initiated. While a cascade of tissue changes typically occurs following an extended duration of penile ischemia, when priapism is reversed prior to 12 hours the patient may maintain some spontaneous erectile ability and or a response to PDE type 5 inhibitors. The non-recoverable nature of the tissue damage because of ischemic priapism at 36 hours is well established.
Based on our extensive review of animal models and clinical reports of ischemic priapism, understanding that many clinical papers used secondary references and espoused concepts out of the dogma, rather than scientific evidence or fact, we believe that a prudent clinician will initiate the reversal of ischemic priapism as early as possible, around the 4-hour mark. The important question that remains largely unanswered to this day, is when does the onset of nonreversible injury first begin in most cases of ischemic priapism? While there does not exist clear evidence in the medical literature to define that timepoint precisely, based on our review of the literature, we believe it is beyond 6 hours and may extend to 12 hours in some men. (Table 1, 2, 3)















