Adamsapple
New Member
Hi all,
Firstly, thanks to Nelson and all on the forum for sharing the breadth of your knowledge online, it's taught and helped me so much. I was hoping I could pick your brains about a specific fertility protocol used by Dr. Ramasamy (interviewed by Nelson on podcast).
Mainly, it is HCG 2000iu EOD with Clomid 50mg.
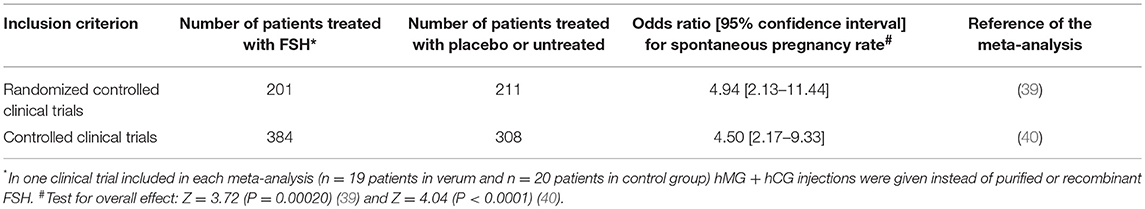
I've read conflicting things about just HCG and SERM being ineffective to restart HPTA with HCG suppressing LH and the effect of this on producing sperm. There are (few) studies that show HCG and Clomid therapy have helped men regain spermatogenesis over the longer term I.e. ramasamy, lipshultz but sperm were deformed in one. It begs the question if HCG supresses FSH production and SERMs can counteract this is anyway?
For background, My wife and I are now trying to get pregnant. I tested azoospermic while on TRT 180mg test E/week in early Feb. I stopped test enanthate on 15 Feb. On 4 March, after test clearing my system- I started Clomid 50mg EOD and Tamoxifen 20mg daily.
I initially started SERMs with HCG, planning to stop HCG and continue with just SERMs. I just had a doctor prescribe me HCG for longer term testosterone maintenance. I am interested but, will using HCG (without HMG) stop me from making sperm , even with alongside serm?
I'm 34 using test on and off since early 20s, have a naturally low test baseline of around 10ng/dl. I'm planning to get to the bottom of why with my endocrinologist but fertility is priority now.
I restarted sperm production after two years on and off, last in 2020 it took 3.5 months for me to get to 10mil sperm count using standard pct and clomid. But that period really took a toll on my personal and professional life. I'm wondering if I can use HCG to help me with sides of SERMs and throughout the PCT. I got bloods done on TRT and have a script ready to check all fertility markers.
I am reaching out because I'm at ends - there is really no option to even get SERMs prescribed by a fertility specialist or Endocrinologist here (both which I'm seeing).
Thanks so much in advance! If anyone is an expert in this area, happy to pay for a consultation over a zoom call.
Firstly, thanks to Nelson and all on the forum for sharing the breadth of your knowledge online, it's taught and helped me so much. I was hoping I could pick your brains about a specific fertility protocol used by Dr. Ramasamy (interviewed by Nelson on podcast).
Mainly, it is HCG 2000iu EOD with Clomid 50mg.
I've read conflicting things about just HCG and SERM being ineffective to restart HPTA with HCG suppressing LH and the effect of this on producing sperm. There are (few) studies that show HCG and Clomid therapy have helped men regain spermatogenesis over the longer term I.e. ramasamy, lipshultz but sperm were deformed in one. It begs the question if HCG supresses FSH production and SERMs can counteract this is anyway?
For background, My wife and I are now trying to get pregnant. I tested azoospermic while on TRT 180mg test E/week in early Feb. I stopped test enanthate on 15 Feb. On 4 March, after test clearing my system- I started Clomid 50mg EOD and Tamoxifen 20mg daily.
I initially started SERMs with HCG, planning to stop HCG and continue with just SERMs. I just had a doctor prescribe me HCG for longer term testosterone maintenance. I am interested but, will using HCG (without HMG) stop me from making sperm , even with alongside serm?
I'm 34 using test on and off since early 20s, have a naturally low test baseline of around 10ng/dl. I'm planning to get to the bottom of why with my endocrinologist but fertility is priority now.
I restarted sperm production after two years on and off, last in 2020 it took 3.5 months for me to get to 10mil sperm count using standard pct and clomid. But that period really took a toll on my personal and professional life. I'm wondering if I can use HCG to help me with sides of SERMs and throughout the PCT. I got bloods done on TRT and have a script ready to check all fertility markers.
I am reaching out because I'm at ends - there is really no option to even get SERMs prescribed by a fertility specialist or Endocrinologist here (both which I'm seeing).
Thanks so much in advance! If anyone is an expert in this area, happy to pay for a consultation over a zoom call.