Hey all, I found out friday my kidneys are in bad shape. I have fanconi syndrome. Basically, I piss all of my minerals out. I have not had a chance to speak to my trt dr. Today is shot day, injust wonder how this effects trt. With adrenal insufficiency, diabetic, this cannot be good.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Fanconi syndrome and TRT
- Thread starter tmckenzie
- Start date
Nelson Vergel
Founder, ExcelMale.com
Tmckensie
I am so sorry to hear. You actually got a diagnosis?
I did a google scholar search and found nothing about testosterone replacement in patients with Fanconi syndrome.
I found this good reference:
The treatment of a child with Fanconi syndrome mainly consists of the replacement of substances lost in the urine. Prominent among these substances are fluids and electrolytes.
Dehydration due to polyuria must be prevented by allowing free access to water; treat dehydration with either oral or parenteral solutions.
Metabolic acidosis due to the loss of bicarbonate is corrected by the administration of alkali, usually 3-10 mg/kg/d of sodium bicarbonate in divided doses.
Addition of a diuretic, such as 1-3 mg/kg/d of hydrochlorothiazide, may be necessary to avoid volume expansion, which magnifies the excretion of bicarbonate by lowering the renal threshold. Unfortunately, the diuretic increases potassium wasting and thus the need to augment potassium supplementation in the form of potassium bicarbonate, citrate, or acetate.
Correction of metabolic acidosis is beneficial but is not sufficient for the treatment of bone disease. Phosphate and vitamin D supplementation are also necessary.
Normalization of serum phosphate levels may be achieved by administering 1-3 g/d of supplemental phosphate. Administration should start at the lower level and be slowly increased over several weeks to minimize GI symptoms.
Vitamin D, administered as 1,25-dihydroxyvitamin D3 or 1a-hydroxyvitamin D3, is preferred because liver and/or renal hydroxylation may be impaired in patients with Fanconi syndrome.
The losses of glucose, amino acids, and uric acid are not usually symptomatic and do not require replacement. Recently, carnitine supplementation has been tried in an attempt to increase muscle strength; however, results have been mixed.
http://emedicine.medscape.com/article/981774-treatment
I am so sorry to hear. You actually got a diagnosis?
I did a google scholar search and found nothing about testosterone replacement in patients with Fanconi syndrome.
I found this good reference:
The treatment of a child with Fanconi syndrome mainly consists of the replacement of substances lost in the urine. Prominent among these substances are fluids and electrolytes.
Dehydration due to polyuria must be prevented by allowing free access to water; treat dehydration with either oral or parenteral solutions.
Metabolic acidosis due to the loss of bicarbonate is corrected by the administration of alkali, usually 3-10 mg/kg/d of sodium bicarbonate in divided doses.
Addition of a diuretic, such as 1-3 mg/kg/d of hydrochlorothiazide, may be necessary to avoid volume expansion, which magnifies the excretion of bicarbonate by lowering the renal threshold. Unfortunately, the diuretic increases potassium wasting and thus the need to augment potassium supplementation in the form of potassium bicarbonate, citrate, or acetate.
Correction of metabolic acidosis is beneficial but is not sufficient for the treatment of bone disease. Phosphate and vitamin D supplementation are also necessary.
Normalization of serum phosphate levels may be achieved by administering 1-3 g/d of supplemental phosphate. Administration should start at the lower level and be slowly increased over several weeks to minimize GI symptoms.
Vitamin D, administered as 1,25-dihydroxyvitamin D3 or 1a-hydroxyvitamin D3, is preferred because liver and/or renal hydroxylation may be impaired in patients with Fanconi syndrome.
The losses of glucose, amino acids, and uric acid are not usually symptomatic and do not require replacement. Recently, carnitine supplementation has been tried in an attempt to increase muscle strength; however, results have been mixed.
http://emedicine.medscape.com/article/981774-treatment
Hi! I have fanconi too, today i realised i piss lots of minerals. How did you treat?Just now looking at my blood work, seems thyroid off too. Tsh was 1.42, free t4 was. .76 range is.61 -1.12. t4 marked low at 3.96 range was 6.09-12.23.
Nelson Vergel
Founder, ExcelMale.com
From AI:
Treatment of Fanconi Syndrome and the Role of Testosterone Replacement Therapy
Overview of Fanconi Syndrome
Fanconi syndrome is a rare disorder characterized by dysfunction of the proximal renal tubules, resulting in the inadequate reabsorption of essential substances that are normally reclaimed by the kidneys [1][2]. This condition leads to excessive loss of glucose, amino acids, phosphate, bicarbonate, uric acid, and other vital electrolytes through urine, causing significant metabolic disturbances [3][4].
The syndrome can be either inherited (primary) or acquired (secondary) through various causes including genetic mutations, drug toxicity, heavy metal exposure, or underlying kidney diseases [2][5]. Cystinosis represents the most common cause of inherited Fanconi syndrome in children, while drug-induced nephrotoxicity accounts for many acquired cases in adults [5][6].
Clinical Manifestations
Inherited Fanconi Syndrome
Children with inherited forms typically present with [7][6]:
Failure to thrive and growth retardation
Polyuria and polydipsia leading to dehydration
Rickets and bone deformities
Muscle weakness and low muscle tone
Corneal abnormalities (in cystinosis cases)
Acquired Fanconi Syndrome
Adults with acquired forms commonly experience [8][6]:
Bone pain and osteomalacia
Muscle weakness
Hypophosphatemia and hypokalemia
Metabolic acidosis
Pathologic fractures
Treatment Approaches for Fanconi Syndrome
Primary Treatment Strategies
The fundamental approach to treating Fanconi syndrome involves addressing the underlying cause when possible and replacing the substances lost through urinary wasting [9][10]. Treatment is primarily supportive and focuses on maintaining metabolic homeostasis.
Fluid and Electrolyte Management
Hydration: Preventing dehydration through adequate fluid intake or intravenous solutions [9][10]
Bicarbonate replacement: Sodium bicarbonate administration (3-15 mEq/kg/day) to correct metabolic acidosis [9][10][11]
Potassium supplementation: Required due to increased urinary losses, typically 20-100 mEq/day in adults [10][11]
Phosphate and Bone Disease Management
Phosphate replacement is crucial for preventing bone complications [9][10][4]:
Phosphate supplementation: 1-3 grams daily of elemental phosphorus, starting with lower doses to minimize gastrointestinal symptoms [9][10]
Active vitamin D: 1,25-dihydroxyvitamin D3 or 1α-hydroxyvitamin D3 preferred due to potential impaired hepatic/renal hydroxylation [9][10]
Calcium supplementation: Often required alongside phosphate and vitamin D therapy [10]
Additional Therapeutic Measures
Thiazide diuretics: May be used to enhance bicarbonate reabsorption and reduce volume expansion, though this increases potassium requirements [9][11]
Dietary modifications: Specific restrictions may be necessary for inherited forms (e.g., limiting fructose in hereditary fructose intolerance) [1][5]
Drug cessation: Discontinuation or dose reduction of nephrotoxic medications when possible [2][11]
Prognosis and Monitoring
The prognosis varies significantly based on the underlying cause [1][10]. Acquired forms may improve with removal of the causative agent, while inherited forms typically require lifelong management [1][8]. Regular monitoring of electrolytes, bone health, and renal function is essential for all patients [9][10].
Testosterone Replacement Therapy in Kidney Disease
TRT in Chronic Kidney Disease
Testosterone replacement therapy has been studied in patients with chronic kidney disease (CKD), where hypogonadism is prevalent [12][13]. Research indicates that up to two-thirds of men on hemodialysis have low testosterone levels, and hypogonadism persists in approximately 25% of renal transplant recipients [14].
Clinical Benefits of TRT in CKD
Studies have demonstrated several potential benefits of TRT in CKD patients [12][13]:
Improved sexual function: Significant enhancement in erectile function scores
Reduced hypogonadal symptoms: Decreased scores on androgen deficiency questionnaires
Potential cardiovascular benefits: Through improved body composition and insulin sensitivity [15]
Enhanced muscle mass and strength: Important for addressing muscle wasting common in CKD [15]
Safety Considerations
Research suggests that TRT may be relatively safe in CKD patients when properly monitored [12][13]. A large retrospective study found that TRT was associated with delayed progression to end-stage renal disease and reduced all-cause mortality [13]. However, careful monitoring for fluid retention and cardiovascular complications remains essential [12][15].
Testosterone and Renal Physiology
Effects on Proximal Tubule Function
Testosterone has complex effects on kidney function, particularly in the proximal tubules where androgen receptors are prominently expressed [16][17][18]. Research has shown that:
Enhanced reabsorption: Testosterone increases proximal tubule volume reabsorption through angiotensin II-mediated mechanisms [17]
Structural effects: Testosterone promotes proximal tubule size and overall kidney growth [16][19]
Transport protein regulation: Androgens modulate expression of key transport proteins including Na/H exchangers [16][17]
Potential Renal Risks
While some studies suggest beneficial effects, concerns exist regarding testosterone's impact on kidney health [20][21]:
Glomerular effects: High-dose or prolonged exposure may promote glomerular injury in some contexts [21]
Apoptotic effects: In vitro studies suggest testosterone may increase susceptibility to proximal tubule cell apoptosis [22]
Blood pressure effects: Testosterone can increase sodium reabsorption and blood pressure [21][17]
TRT Considerations in Fanconi Syndrome
Theoretical Interactions
Given that Fanconi syndrome specifically involves proximal tubule dysfunction and testosterone primarily affects proximal tubule transport and structure, several theoretical considerations emerge:
Potential Benefits
Enhanced tubular function: Testosterone's ability to increase proximal tubule reabsorption might theoretically improve some aspects of tubular dysfunction [17]
Structural support: Testosterone's effects on proximal tubule size and cellular integrity could potentially provide some benefit [16][19]
Potential Risks
Increased metabolic demands: Enhanced proximal tubule activity might worsen existing dysfunction in compromised tubules
Electrolyte imbalances: Testosterone's effects on sodium and water reabsorption could complicate fluid and electrolyte management [17]
Cellular stress: Given testosterone's potential apoptotic effects on proximal tubule cells, this could theoretically worsen tubular damage [22]
Clinical Recommendations
Currently, there is insufficient specific research on TRT use in patients with Fanconi syndrome. However, based on available evidence:
When TRT Might Be Considered
Patients with clear hypogonadism and significant symptoms affecting quality of life
Cases where the underlying cause of Fanconi syndrome is stable or improving
Patients with adequate kidney function reserves
Precautions and Monitoring
If TRT is considered in Fanconi syndrome patients, enhanced monitoring would be essential:
Frequent electrolyte assessment: Given the complex interactions with proximal tubule transport
Renal function monitoring: Regular assessment of GFR and tubular function markers
Bone health evaluation: Careful monitoring of phosphate, calcium, and bone metabolism parameters
Fluid status assessment: Watching for signs of fluid retention or cardiovascular complications
Conclusion
The treatment of Fanconi syndrome remains primarily supportive, focusing on replacement of lost substances and management of metabolic complications [1][9][10]. While testosterone replacement therapy has shown promise in chronic kidney disease patients, its specific role in Fanconi syndrome requires further investigation [12][13].
The complex interactions between testosterone and proximal tubule function suggest both potential benefits and risks in Fanconi syndrome patients [16][17]. Any consideration of TRT in this population should involve careful risk-benefit analysis, close monitoring, and coordination between nephrology and endocrinology specialists [15].
Future research specifically examining TRT outcomes in Fanconi syndrome patients would be valuable to establish evidence-based guidelines for this complex clinical scenario. Until such data becomes available, individualized decision-making with comprehensive monitoring remains the most prudent approach.
Fanconi Syndrome: Causes, Symptoms & Treatment
Fanconi Syndrome - Genitourinary Disorders - Merck Manual Professional Edition
Fanconi syndrome - Wikipedia
Fanconi Syndrome.
Fanconi syndrome Information | Mount Sinai - New York
Fanconi Syndrome: Symptoms, Causes, Treatment, and Outlook
Fanconi Syndrome: Practice Essentials, Background, Pathophysiology
Fanconi Syndrome - Kidney and Urinary Tract Disorders - Merck Manual Consumer Version
Fanconi Syndrome Treatment & Management: Medical Care, Surgical Care, Consultations
Fanconi syndrome in the adulthood. The role of early diagnosis and treatment - PMC
Proximal renal tubular acidosis with and without Fanconi syndrome - PMC
Testosterone Replacement Therapy in Chronic Kidney Disease Patients - PMC
Testosterone Replacement Therapy (TRT) is Associated with Delayed Progression of Chronic Kidney Disease: A Retrospective Analysis of Testosterone Normalization in US Veterans
A case series of the safety and efficacy of testosterone replacement therapy in renal failure and kidney transplant patients - Majzoub - Translational Andrology and Urology
Testosterone deficiency and chronic kidney disease - PubMed
https://journals.physiology.org/doi/abs/10.1152/ajprenal.00560.2019
https://journals.physiology.org/doi/10.1152/ajprenal.00188.2003
https://pmc.ncbi.nlm.nih.gov/articles/PMC8616601/
https://pmc.ncbi.nlm.nih.gov/articles/PMC7191448/
https://pmc.ncbi.nlm.nih.gov/articles/PMC5720528/
https://www.ahajournals.org/doi/10.1161/hypertensionaha.107.105767
https://pubmed.ncbi.nlm.nih.gov/15086464/
Treatment of Fanconi Syndrome and the Role of Testosterone Replacement Therapy
Overview of Fanconi Syndrome
Fanconi syndrome is a rare disorder characterized by dysfunction of the proximal renal tubules, resulting in the inadequate reabsorption of essential substances that are normally reclaimed by the kidneys [1][2]. This condition leads to excessive loss of glucose, amino acids, phosphate, bicarbonate, uric acid, and other vital electrolytes through urine, causing significant metabolic disturbances [3][4].
The syndrome can be either inherited (primary) or acquired (secondary) through various causes including genetic mutations, drug toxicity, heavy metal exposure, or underlying kidney diseases [2][5]. Cystinosis represents the most common cause of inherited Fanconi syndrome in children, while drug-induced nephrotoxicity accounts for many acquired cases in adults [5][6].
Clinical Manifestations
Inherited Fanconi Syndrome
Children with inherited forms typically present with [7][6]:
Failure to thrive and growth retardation
Polyuria and polydipsia leading to dehydration
Rickets and bone deformities
Muscle weakness and low muscle tone
Corneal abnormalities (in cystinosis cases)
Acquired Fanconi Syndrome
Adults with acquired forms commonly experience [8][6]:
Bone pain and osteomalacia
Muscle weakness
Hypophosphatemia and hypokalemia
Metabolic acidosis
Pathologic fractures
Treatment Approaches for Fanconi Syndrome
Primary Treatment Strategies
The fundamental approach to treating Fanconi syndrome involves addressing the underlying cause when possible and replacing the substances lost through urinary wasting [9][10]. Treatment is primarily supportive and focuses on maintaining metabolic homeostasis.
Fluid and Electrolyte Management
Hydration: Preventing dehydration through adequate fluid intake or intravenous solutions [9][10]
Bicarbonate replacement: Sodium bicarbonate administration (3-15 mEq/kg/day) to correct metabolic acidosis [9][10][11]
Potassium supplementation: Required due to increased urinary losses, typically 20-100 mEq/day in adults [10][11]
Phosphate and Bone Disease Management
Phosphate replacement is crucial for preventing bone complications [9][10][4]:
Phosphate supplementation: 1-3 grams daily of elemental phosphorus, starting with lower doses to minimize gastrointestinal symptoms [9][10]
Active vitamin D: 1,25-dihydroxyvitamin D3 or 1α-hydroxyvitamin D3 preferred due to potential impaired hepatic/renal hydroxylation [9][10]
Calcium supplementation: Often required alongside phosphate and vitamin D therapy [10]
Additional Therapeutic Measures
Thiazide diuretics: May be used to enhance bicarbonate reabsorption and reduce volume expansion, though this increases potassium requirements [9][11]
Dietary modifications: Specific restrictions may be necessary for inherited forms (e.g., limiting fructose in hereditary fructose intolerance) [1][5]
Drug cessation: Discontinuation or dose reduction of nephrotoxic medications when possible [2][11]
Prognosis and Monitoring
The prognosis varies significantly based on the underlying cause [1][10]. Acquired forms may improve with removal of the causative agent, while inherited forms typically require lifelong management [1][8]. Regular monitoring of electrolytes, bone health, and renal function is essential for all patients [9][10].
Testosterone Replacement Therapy in Kidney Disease
TRT in Chronic Kidney Disease
Testosterone replacement therapy has been studied in patients with chronic kidney disease (CKD), where hypogonadism is prevalent [12][13]. Research indicates that up to two-thirds of men on hemodialysis have low testosterone levels, and hypogonadism persists in approximately 25% of renal transplant recipients [14].
Clinical Benefits of TRT in CKD
Studies have demonstrated several potential benefits of TRT in CKD patients [12][13]:
Improved sexual function: Significant enhancement in erectile function scores
Reduced hypogonadal symptoms: Decreased scores on androgen deficiency questionnaires
Potential cardiovascular benefits: Through improved body composition and insulin sensitivity [15]
Enhanced muscle mass and strength: Important for addressing muscle wasting common in CKD [15]
Safety Considerations
Research suggests that TRT may be relatively safe in CKD patients when properly monitored [12][13]. A large retrospective study found that TRT was associated with delayed progression to end-stage renal disease and reduced all-cause mortality [13]. However, careful monitoring for fluid retention and cardiovascular complications remains essential [12][15].
Testosterone and Renal Physiology
Effects on Proximal Tubule Function
Testosterone has complex effects on kidney function, particularly in the proximal tubules where androgen receptors are prominently expressed [16][17][18]. Research has shown that:
Enhanced reabsorption: Testosterone increases proximal tubule volume reabsorption through angiotensin II-mediated mechanisms [17]
Structural effects: Testosterone promotes proximal tubule size and overall kidney growth [16][19]
Transport protein regulation: Androgens modulate expression of key transport proteins including Na/H exchangers [16][17]
Potential Renal Risks
While some studies suggest beneficial effects, concerns exist regarding testosterone's impact on kidney health [20][21]:
Glomerular effects: High-dose or prolonged exposure may promote glomerular injury in some contexts [21]
Apoptotic effects: In vitro studies suggest testosterone may increase susceptibility to proximal tubule cell apoptosis [22]
Blood pressure effects: Testosterone can increase sodium reabsorption and blood pressure [21][17]
TRT Considerations in Fanconi Syndrome
Theoretical Interactions
Given that Fanconi syndrome specifically involves proximal tubule dysfunction and testosterone primarily affects proximal tubule transport and structure, several theoretical considerations emerge:
Potential Benefits
Enhanced tubular function: Testosterone's ability to increase proximal tubule reabsorption might theoretically improve some aspects of tubular dysfunction [17]
Structural support: Testosterone's effects on proximal tubule size and cellular integrity could potentially provide some benefit [16][19]
Potential Risks
Increased metabolic demands: Enhanced proximal tubule activity might worsen existing dysfunction in compromised tubules
Electrolyte imbalances: Testosterone's effects on sodium and water reabsorption could complicate fluid and electrolyte management [17]
Cellular stress: Given testosterone's potential apoptotic effects on proximal tubule cells, this could theoretically worsen tubular damage [22]
Clinical Recommendations
Currently, there is insufficient specific research on TRT use in patients with Fanconi syndrome. However, based on available evidence:
When TRT Might Be Considered
Patients with clear hypogonadism and significant symptoms affecting quality of life
Cases where the underlying cause of Fanconi syndrome is stable or improving
Patients with adequate kidney function reserves
Precautions and Monitoring
If TRT is considered in Fanconi syndrome patients, enhanced monitoring would be essential:
Frequent electrolyte assessment: Given the complex interactions with proximal tubule transport
Renal function monitoring: Regular assessment of GFR and tubular function markers
Bone health evaluation: Careful monitoring of phosphate, calcium, and bone metabolism parameters
Fluid status assessment: Watching for signs of fluid retention or cardiovascular complications
Conclusion
The treatment of Fanconi syndrome remains primarily supportive, focusing on replacement of lost substances and management of metabolic complications [1][9][10]. While testosterone replacement therapy has shown promise in chronic kidney disease patients, its specific role in Fanconi syndrome requires further investigation [12][13].
The complex interactions between testosterone and proximal tubule function suggest both potential benefits and risks in Fanconi syndrome patients [16][17]. Any consideration of TRT in this population should involve careful risk-benefit analysis, close monitoring, and coordination between nephrology and endocrinology specialists [15].
Future research specifically examining TRT outcomes in Fanconi syndrome patients would be valuable to establish evidence-based guidelines for this complex clinical scenario. Until such data becomes available, individualized decision-making with comprehensive monitoring remains the most prudent approach.
Fanconi Syndrome: Causes, Symptoms & Treatment
Fanconi Syndrome - Genitourinary Disorders - Merck Manual Professional Edition
Fanconi syndrome - Wikipedia
Fanconi Syndrome.
Fanconi syndrome Information | Mount Sinai - New York
Fanconi Syndrome: Symptoms, Causes, Treatment, and Outlook
Fanconi Syndrome: Practice Essentials, Background, Pathophysiology
Fanconi Syndrome - Kidney and Urinary Tract Disorders - Merck Manual Consumer Version
Fanconi Syndrome Treatment & Management: Medical Care, Surgical Care, Consultations
Fanconi syndrome in the adulthood. The role of early diagnosis and treatment - PMC
Proximal renal tubular acidosis with and without Fanconi syndrome - PMC
Testosterone Replacement Therapy in Chronic Kidney Disease Patients - PMC
Testosterone Replacement Therapy (TRT) is Associated with Delayed Progression of Chronic Kidney Disease: A Retrospective Analysis of Testosterone Normalization in US Veterans
A case series of the safety and efficacy of testosterone replacement therapy in renal failure and kidney transplant patients - Majzoub - Translational Andrology and Urology
Testosterone deficiency and chronic kidney disease - PubMed
https://journals.physiology.org/doi/abs/10.1152/ajprenal.00560.2019
https://journals.physiology.org/doi/10.1152/ajprenal.00188.2003
https://pmc.ncbi.nlm.nih.gov/articles/PMC8616601/
https://pmc.ncbi.nlm.nih.gov/articles/PMC7191448/
https://pmc.ncbi.nlm.nih.gov/articles/PMC5720528/
https://www.ahajournals.org/doi/10.1161/hypertensionaha.107.105767
https://pubmed.ncbi.nlm.nih.gov/15086464/
Nelson Vergel
Founder, ExcelMale.com
Best Electrolyte Products for Treating Fanconi Syndrome
Overview of Electrolyte Needs in Fanconi Syndrome
Fanconi syndrome leads to the excessive loss of key electrolytes and nutrients—including sodium, potassium, phosphate, bicarbonate, and others—due to impaired reabsorption in the renal proximal tubules[1][2][3]. Treatment focuses on replacing these lost electrolytes and correcting acid-base imbalances to prevent complications such as dehydration, metabolic acidosis, bone disease, and muscle weakness[4][5][6][2].
Key Electrolytes and Supplements Commonly Needed
· Potassium (often as potassium chloride or potassium citrate)
· Phosphate (as sodium or potassium phosphate)
· Bicarbonate (as sodium bicarbonate or potassium citrate)
· Calcium and Vitamin D (especially if bone health is compromised)
· Other minerals and multivitamins (as needed for overall nutritional support)
Best Electrolyte Product Types
The best products are those that provide targeted, titratable doses of the specific electrolytes lost, ideally available in oral formulations for chronic management. Here are commonly recommended product types:
1. Potassium Supplements
· Potassium Chloride Tablets/Capsules (e.g., Klor-Con, Micro-K)
· Potassium Citrate Tablets (e.g., Urocit-K, Cytra-K; also provides bicarbonate equivalents)[6][2]
· Oral solutions (for those with swallowing difficulties)
2. Phosphate Supplements
· Sodium Phosphate or Potassium Phosphate Tablets/Powders (e.g., Neutra-Phos, K-Phos)
· Dosed based on serum phosphate levels and GI tolerance[6][2]
3. Bicarbonate Supplements
· Sodium Bicarbonate Tablets or Powder
· Potassium Citrate (as above, also provides bicarbonate)[6][2][7]
4. Calcium and Vitamin D
· Calcium Carbonate Tablets
· Active Vitamin D (calcitriol) if indicated[2]
5. Oral Electrolyte Solutions
· Rehydration solutions (e.g., Pedialyte, generic oral rehydration salts)
· Custom-compounded electrolyte mixes (by prescription)
6. Multivitamins and Amino Acid Supplements
· Comprehensive multivitamins (e.g., Centrum, as sometimes recommended in veterinary protocols)[8]
· Amino acid supplements if there is evidence of deficiency
Where to Buy These Electrolyte Products
· Major Pharmacies: CVS, Walgreens, Walmart, Rite Aid, and Target pharmacies typically stock potassium chloride, sodium bicarbonate, calcium carbonate, and multivitamins. Ask the pharmacist for prescription-strength phosphate or potassium citrate products.
· Online Pharmacies: Websites like Amazon, HealthWarehouse, and pharmacy chains' online stores often carry over-the-counter forms of these supplements.
· Medical Supply Stores: Some specialized products (like oral phosphate powders or compounded electrolyte solutions) may be available through medical supply companies or with a prescription from a compounding pharmacy.
· Prescription Required: Many higher-dose or specific formulations (e.g., potassium phosphate, potassium citrate, Neutra-Phos, Urocit-K) require a prescription from a healthcare provider[6][2][9].
Important Considerations
· Dosing and Monitoring: Electrolyte replacement must be individualized and closely monitored by a healthcare provider, with regular blood tests to avoid over- or under-correction, especially for potassium and phosphate[6][2][9].
· Consultation: Always consult your physician or a nephrologist before starting or adjusting any electrolyte supplement regimen for Fanconi syndrome.
Summary Table: Common Electrolyte Supplements for Fanconi Syndrome
Note: Always use these products under medical supervision to ensure safety and efficacy[6][2][9].
In summary:
The best electrolyte products for treating Fanconi syndrome are prescription and over-the-counter potassium, phosphate, and bicarbonate supplements, along with calcium, vitamin D, and multivitamins as needed. These are widely available at major pharmacies and online retailers, but dosing and monitoring should always be managed by a healthcare provider due to the complexity and risks associated with electrolyte replacement in Fanconi syndrome[6][2][9].
1. https://www.healthline.com/health/fanconi-syndrome
2. https://pmc.ncbi.nlm.nih.gov/articles/PMC5749037/
3. https://vcahospitals.com/know-your-pet/fanconi-syndrome-in-dogs
4. https://emedicine.medscape.com/article/981774-treatment
5. https://www.ncbi.nlm.nih.gov/books/NBK534872/
6. https://www.uspharmacist.com/article/fanconi-syndrome
7. https://www.basenjirescue.org/Fanconi/fanconi.asp
8. https://vetfolio.s3.amazonaws.com/0b/70/98962ecf45afac539a272790c25f/fanconi-syndrome-pdf.pdf
9. https://my.clevelandclinic.org/health/diseases/24233-fanconi-syndrome
Overview of Electrolyte Needs in Fanconi Syndrome
Fanconi syndrome leads to the excessive loss of key electrolytes and nutrients—including sodium, potassium, phosphate, bicarbonate, and others—due to impaired reabsorption in the renal proximal tubules[1][2][3]. Treatment focuses on replacing these lost electrolytes and correcting acid-base imbalances to prevent complications such as dehydration, metabolic acidosis, bone disease, and muscle weakness[4][5][6][2].
Key Electrolytes and Supplements Commonly Needed
· Potassium (often as potassium chloride or potassium citrate)
· Phosphate (as sodium or potassium phosphate)
· Bicarbonate (as sodium bicarbonate or potassium citrate)
· Calcium and Vitamin D (especially if bone health is compromised)
· Other minerals and multivitamins (as needed for overall nutritional support)
Best Electrolyte Product Types
The best products are those that provide targeted, titratable doses of the specific electrolytes lost, ideally available in oral formulations for chronic management. Here are commonly recommended product types:
1. Potassium Supplements
· Potassium Chloride Tablets/Capsules (e.g., Klor-Con, Micro-K)
· Potassium Citrate Tablets (e.g., Urocit-K, Cytra-K; also provides bicarbonate equivalents)[6][2]
· Oral solutions (for those with swallowing difficulties)
2. Phosphate Supplements
· Sodium Phosphate or Potassium Phosphate Tablets/Powders (e.g., Neutra-Phos, K-Phos)
· Dosed based on serum phosphate levels and GI tolerance[6][2]
3. Bicarbonate Supplements
· Sodium Bicarbonate Tablets or Powder
· Potassium Citrate (as above, also provides bicarbonate)[6][2][7]
4. Calcium and Vitamin D
· Calcium Carbonate Tablets
· Active Vitamin D (calcitriol) if indicated[2]
5. Oral Electrolyte Solutions
· Rehydration solutions (e.g., Pedialyte, generic oral rehydration salts)
· Custom-compounded electrolyte mixes (by prescription)
6. Multivitamins and Amino Acid Supplements
· Comprehensive multivitamins (e.g., Centrum, as sometimes recommended in veterinary protocols)[8]
· Amino acid supplements if there is evidence of deficiency
Where to Buy These Electrolyte Products
· Major Pharmacies: CVS, Walgreens, Walmart, Rite Aid, and Target pharmacies typically stock potassium chloride, sodium bicarbonate, calcium carbonate, and multivitamins. Ask the pharmacist for prescription-strength phosphate or potassium citrate products.
· Online Pharmacies: Websites like Amazon, HealthWarehouse, and pharmacy chains' online stores often carry over-the-counter forms of these supplements.
· Medical Supply Stores: Some specialized products (like oral phosphate powders or compounded electrolyte solutions) may be available through medical supply companies or with a prescription from a compounding pharmacy.
· Prescription Required: Many higher-dose or specific formulations (e.g., potassium phosphate, potassium citrate, Neutra-Phos, Urocit-K) require a prescription from a healthcare provider[6][2][9].
Important Considerations
· Dosing and Monitoring: Electrolyte replacement must be individualized and closely monitored by a healthcare provider, with regular blood tests to avoid over- or under-correction, especially for potassium and phosphate[6][2][9].
· Consultation: Always consult your physician or a nephrologist before starting or adjusting any electrolyte supplement regimen for Fanconi syndrome.
Summary Table: Common Electrolyte Supplements for Fanconi Syndrome
Electrolyte | Example Products | OTC or Rx | Where to Buy |
Potassium | Klor-Con, Urocit-K | Rx | Pharmacy, online pharmacy |
Phosphate | Neutra-Phos, K-Phos | Rx | Pharmacy, online pharmacy |
Bicarbonate | Sodium bicarbonate tabs | OTC/Rx | Pharmacy, online, supermarkets |
Calcium/Vitamin D | Caltrate, Calcitriol | OTC/Rx | Pharmacy, online |
Multivitamin | Centrum, One-A-Day | OTC | Pharmacy, supermarket, online |
Oral Solutions | Pedialyte, generic ORS | OTC | Pharmacy, supermarket, online |
Note: Always use these products under medical supervision to ensure safety and efficacy[6][2][9].
In summary:
The best electrolyte products for treating Fanconi syndrome are prescription and over-the-counter potassium, phosphate, and bicarbonate supplements, along with calcium, vitamin D, and multivitamins as needed. These are widely available at major pharmacies and online retailers, but dosing and monitoring should always be managed by a healthcare provider due to the complexity and risks associated with electrolyte replacement in Fanconi syndrome[6][2][9].
1. https://www.healthline.com/health/fanconi-syndrome
2. https://pmc.ncbi.nlm.nih.gov/articles/PMC5749037/
3. https://vcahospitals.com/know-your-pet/fanconi-syndrome-in-dogs
4. https://emedicine.medscape.com/article/981774-treatment
5. https://www.ncbi.nlm.nih.gov/books/NBK534872/
6. https://www.uspharmacist.com/article/fanconi-syndrome
7. https://www.basenjirescue.org/Fanconi/fanconi.asp
8. https://vetfolio.s3.amazonaws.com/0b/70/98962ecf45afac539a272790c25f/fanconi-syndrome-pdf.pdf
9. https://my.clevelandclinic.org/health/diseases/24233-fanconi-syndrome
Nelson Vergel
Founder, ExcelMale.com
Could These Lab Test Values Indicate Fanconi Syndrome?
I notice you've asked about lab test values that might indicate Fanconi syndrome, but I don't see any specific lab results provided in your query. However, I can provide you with comprehensive information about the characteristic laboratory findings that are diagnostic for Fanconi syndrome, which will help you evaluate any test results you may have.What is Fanconi Syndrome?
Fanconi syndrome is a disorder of inadequate reabsorption in the proximal renal tubules of the kidney, resulting in various small molecules being passed into the urine instead of being reabsorbed9. The syndrome consists of multiple defects in renal proximal tubular reabsorption, causing glucosuria, phosphaturia, generalized aminoaciduria, and bicarbonate wasting8. It can be either hereditary or acquired, with acquired forms often caused by medications, heavy metals, or other toxic substances13.Key Laboratory Findings for Fanconi Syndrome Diagnosis
Primary Diagnostic Criteria
The diagnosis of Fanconi syndrome is made based on tests that document the excessive loss of substances in the urine in the absence of high plasma concentrations1. The most important laboratory findings include:Glucosuria with Normal Blood Glucose
- High levels of glucose in urine despite normal or low blood glucose levels23
- This glucose disconnect is often the very first suggestion of Fanconi syndrome23
- Normally, urine contains very little or no glucose21
- Excessive phosphate loss in urine28
- Often accompanied by hypophosphatemia (low blood phosphate levels)2
- Normal serum phosphate ranges from 2.5-4.5 mg/dL7
- Excessive amino acids of all classes in urine18
- This represents a broad-spectrum loss rather than specific amino acid defects22
- Fractional bicarbonate excretion >15% clearly establishes proximal renal tubular acidosis13
- Even fractional bicarbonate excretion above 5% may be sufficient for diagnosis of less severe types13
- Results in type 2 (proximal) renal tubular acidosis7
Additional Laboratory Abnormalities
Electrolyte Imbalances- Hypokalemia (low potassium levels)26
- Hyponatremia and hypochloremia may occur622
- Metabolic acidosis with normal anion gap716
- Proteinuria (protein in urine)212
- Hyperuricosuria (excessive uric acid in urine)913
- Hypercalciuria (excessive calcium in urine) may be present6
- Low serum bicarbonate levels (normal range 22-26 mmol/L)67
- Elevated anion gap may be present6
- Normal or slightly elevated creatinine depending on kidney function6
Diagnostic Approach
Confirming the Diagnosis
Healthcare providers typically order both urine and blood tests2. The combination of urine glucose with normal or low blood glucose strongly suggests Fanconi syndrome11. High levels of glucose, amino acids, and phosphates in urine help confirm the diagnosis, while low blood levels of phosphate, bicarbonate, and potassium may also indicate the condition2.Specialized Testing
More elaborate tests can determine the renal threshold for various substances or their fractional reabsorption1. Recently, an increased urinary lactate-to-creatinine ratio has been proposed as a sensitive test for disordered proximal tubular function1. Additionally, urinary retinol-binding protein 4 appears to be an excellent screening test for Fanconi syndrome1.Differential Diagnosis Considerations
It's important to distinguish Fanconi syndrome from other conditions that may present with similar laboratory findings14:- Diabetes mellitus: Would show elevated blood glucose along with glucosuria
- Isolated renal glucosuria: Shows only glucose wasting without other tubular defects1517
- Other renal tubular acidoses: Different patterns of electrolyte abnormalities14
- Nephrotic syndrome: Would show hypoproteinemia and hyperlipidemia14
Clinical Significance
The clinical features that typically accompany these laboratory findings include polyuria, polydipsia, failure to thrive in children, bone pain and weakness in adults, and episodes of dehydration5. In children, the condition often presents with growth retardation and rickets, while adults may develop osteomalacia and muscle weakness8.Conclusion
If you have specific lab results that show glucosuria with normal blood glucose, along with evidence of phosphate wasting, amino acid excretion, and metabolic acidosis, these findings would be highly suggestive of Fanconi syndrome123. However, a comprehensive evaluation by a nephrologist would be essential for definitive diagnosis and to determine the underlying cause, whether hereditary or acquired2.Thanks for the replying. Nephrologist dont know too much about it, because i went to other and said me everything is right. But i have lot of Weirds symptons, like muscular fatigue, kidney pain and dizziness. Labs shows minerals Wasting like phosphate and pottasium. It seems there is a tubular atrophy, and in reading about protocolos to heal myself.
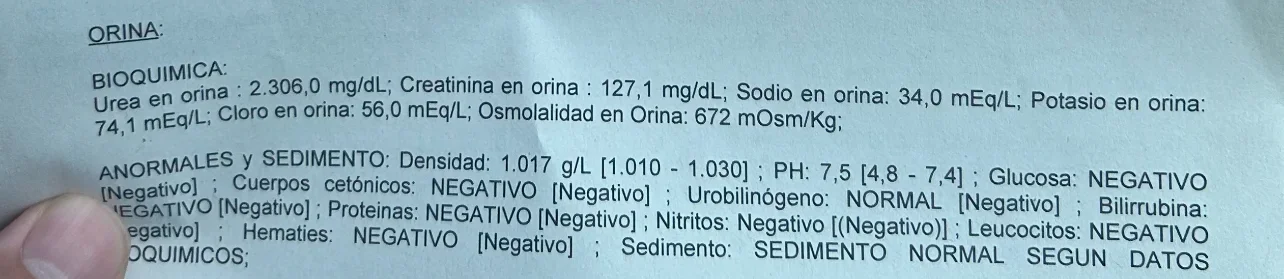
First one is the 24hour excretion and the second an isolated sample
First one is the 24hour excretion and the second an isolated sample
Attachments
Nelson Vergel
Founder, ExcelMale.com
Based on an AI analysis:
Based on this 24-hour urine analysis, several parameters show significant abnormalities that warrant clinical attention:
The total protein excretion of 168.8 mg/24h exceeds the normal range (0-140 mg/24h) and indicates proteinuria12. While not severely elevated, this level suggests early kidney dysfunction or damage to the glomerular filtration system1.
Polyuria (Excessive Urine Volume)
The urine volume of 3,350 mL/24h is significantly elevated, nearly double the upper normal limit of 1,800 mL/24h34. Normal 24-hour urine output ranges from 800-2,000 mL/day with typical fluid intake4. This polyuria could indicate diabetes mellitus, diabetes insipidus, or excessive fluid intake4.
Elevated Creatinine Excretion
At 3.68 g/24h, creatinine excretion substantially exceeds normal ranges (males: 0.8-1.8 g/day, females: 0.6-1.6 g/day)56. This elevation, combined with the high urine volume, suggests increased muscle metabolism or potential kidney dysfunction.
Significantly Elevated Urea Excretion
The urea excretion of 72.8 g/24h is markedly elevated compared to the normal range of 26-43 g/24h7. This indicates increased protein breakdown in the body or excessive protein intake7.
Elevated Uric Acid Excretion
At 1,614.7 mg/24h, uric acid excretion is more than double the normal range of 250-750 mg/24h. This suggests increased purine metabolism or dietary purine intake8.
Elevated Phosphorus Excretion
The phosphorus excretion of 2,452.2 mg/24h significantly exceeds the normal range of 400-1,300 mg/24h9. This could indicate increased dietary phosphorus intake or altered phosphorus metabolism.
At 10.05 mg/24h, microalbumin levels are well within the normal range (<30 mg/24h)1011, indicating no evidence of early diabetic nephropathy or vascular disease.
Calcium Excretion
The calcium excretion of 294.1 mg/24h falls within the normal range of 100-300 mg/24h1213, suggesting normal calcium metabolism and no increased kidney stone risk from hypercalciuria.
Magnesium Excretion
At 196.6 mg/24h, magnesium excretion is within the normal range of 24-210 mg/24h14, indicating adequate magnesium status.
Based on this 24-hour urine analysis, several parameters show significant abnormalities that warrant clinical attention:
Abnormal Findings
Elevated Protein ExcretionThe total protein excretion of 168.8 mg/24h exceeds the normal range (0-140 mg/24h) and indicates proteinuria12. While not severely elevated, this level suggests early kidney dysfunction or damage to the glomerular filtration system1.
Polyuria (Excessive Urine Volume)
The urine volume of 3,350 mL/24h is significantly elevated, nearly double the upper normal limit of 1,800 mL/24h34. Normal 24-hour urine output ranges from 800-2,000 mL/day with typical fluid intake4. This polyuria could indicate diabetes mellitus, diabetes insipidus, or excessive fluid intake4.
Elevated Creatinine Excretion
At 3.68 g/24h, creatinine excretion substantially exceeds normal ranges (males: 0.8-1.8 g/day, females: 0.6-1.6 g/day)56. This elevation, combined with the high urine volume, suggests increased muscle metabolism or potential kidney dysfunction.
Significantly Elevated Urea Excretion
The urea excretion of 72.8 g/24h is markedly elevated compared to the normal range of 26-43 g/24h7. This indicates increased protein breakdown in the body or excessive protein intake7.
Elevated Uric Acid Excretion
At 1,614.7 mg/24h, uric acid excretion is more than double the normal range of 250-750 mg/24h. This suggests increased purine metabolism or dietary purine intake8.
Elevated Phosphorus Excretion
The phosphorus excretion of 2,452.2 mg/24h significantly exceeds the normal range of 400-1,300 mg/24h9. This could indicate increased dietary phosphorus intake or altered phosphorus metabolism.
Normal Findings
Microalbumin ExcretionAt 10.05 mg/24h, microalbumin levels are well within the normal range (<30 mg/24h)1011, indicating no evidence of early diabetic nephropathy or vascular disease.
Calcium Excretion
The calcium excretion of 294.1 mg/24h falls within the normal range of 100-300 mg/24h1213, suggesting normal calcium metabolism and no increased kidney stone risk from hypercalciuria.
Magnesium Excretion
At 196.6 mg/24h, magnesium excretion is within the normal range of 24-210 mg/24h14, indicating adequate magnesium status.
Clinical Implications
The pattern of elevated protein excretion combined with polyuria suggests possible kidney dysfunction that requires further evaluation. The significantly elevated excretion of multiple waste products (urea, uric acid, phosphorus) along with increased urine volume may indicate:- Diabetes mellitus - particularly given the polyuria
- Early kidney disease - evidenced by proteinuria
- Metabolic disorders affecting protein and purine metabolism
- Dietary factors - high protein or purine intake
Nelson Vergel
Founder, ExcelMale.com
Nelson Vergel
Founder, ExcelMale.com
Visión general
El informe corresponde a una recolección urinaria de 24 horas. Para cada analito indico:| Parámetro | Resultado | Intervalo de referencia del laboratorio | Interpretación breve |
|---|---|---|---|
| Volumen (diuresis) | 3 350 mL/24 h | 600 – 1 800 | Poliuria leve; suele reflejar alta ingesta de líquidos, uso de diuréticos o hiperglucemia/osmótica. |
| Proteínas – concentración | 5 mg/dL | — | Dato orientativo; lo relevante es la excreción total. |
| Proteínas – excreción | 168.8 mg/24 h | 0 – 140 | Proteinuria leve (no nefrótica). Compatible con proteinuria tubular, transitoria (fiebre, ejercicio) o inicial glomerular. |
| Microalbúmina – concentración | 3.0 mg/L | — | Normal. |
| Microalbúmina – excreción | 10.05 mg/24 h | 0 – 30 | Dentro de rango; descarta microalbuminuria (útil para despistaje de nefropatía diabética/HTA). |
| Creatinina – concentración | 110 mg/dL | — | Normal. |
| Creatinina – excreción | 3.68 g/24 h | 1.04 – 2.35 | Superior al rango: puede indicar colección completa en persona con elevada masa muscular o una ingesta proteica alta; ocasionalmente sugiere sobre‑recolección (>24 h). |
| Urea – concentración | 2 172 mg/dL | — | — |
| Urea – excreción | 72.8 g/24 h | 25.7 – 42.9 | Muy elevada: orienta a dieta rica en proteínas o catabolismo aumentado. |
| Ácido úrico – concentración | 48.2 mg/dL | — | — |
| Ácido úrico – excreción | 1 614.7 mg/24 h | 250 – 750 | Hiperuricosuria. Incrementa riesgo de litiasis de ácido úrico o mixtas. Relacionado con dieta (carnes rojas, vísceras), síndromes mielo‑proliferativos, exceso de fructosa, resistencia a insulina. |
| Calcio – concentración | 8.8 mg/dL | — | — |
| Calcio – excreción | 294.1 mg/24 h | 100 – 300 | En el límite alto (hipercalciuria limítrofe). Junto con urato alto eleva riesgo litiásico. |
| Fósforo – concentración | 73.2 mg/dL | — | — |
| Fósforo – excreción | 2 452.2 mg/24 h | 400 – 1 300 | Hiperfosfaturia. Suele deberse a ingesta alta (bebidas cola, alimentos procesados) o hiperparatiroidismo secundario a alta carga proteica/fosfórica. |
| Magnesio – concentración | 5.9 mg/dL | — | — |
| Magnesio – excreción | 196.6 mg/24 h | 24 – 210 | Normal‑alto; el magnesio es litoinhibidor, por lo que este dato es favorable. |
| Citrato – excreción | Pendiente | — | El citrato es un inhibidor de la formación de cálculos; será clave conocerlo. |
Interpretación clínica integrada
- Perfil de alto aporte proteico
- Urea y fósforo muy elevados, junto con creatinina y volumen total altos, sugieren dieta rica en proteínas animales y fosfatos.
- Esto explica en parte la proteinuria leve y la hiperuricosuria.
- Riesgo metabólico para litiasis renal
- Hiperuricosuria + hiperfosfaturia + calcio alto‑normal y un citrato aún desconocido configuran un terreno propenso a la formación de cálculos (urato, oxalato/cálcico mixtos).
- La orina abundantemente diluida (3.3 L) es protectora, pero el exceso de solutos puede contrarrestar ese beneficio.
- Función renal global
- La ausencia de microalbuminuria y la proteinuria <300 mg/24 h indican que, por ahora, no hay lesión glomerular significativa.
- Creatinina urinaria alta sugiere buena filtración o simplemente mayor producción muscular; habría que correlacionar con creatinina sérica.
- Posible sobre‑recolección (o alta masa muscular)
- Creatinina 3.68 g/24 h está por encima del máximo habitual (≈25 mg/kg/día en varones). Si el peso corporal es bajo o medio, conviene verificar que la muestra abarque exactamente 24 h.
Próximos pasos y recomendaciones (a discutir con su médico)
| Área | Acción recomendada | Justificación |
|---|---|---|
| Confirmar recolección | Revisar instrucciones, considerar repetir 24 h si peso corporal no justifica 3.6 g creatinina | Asegurar validez cuantitativa de todos los analitos. |
| Analítica sérica | Creatinina, ácido úrico, fósforo, calcio, PTH | Correlación con hallazgos urinarios y función renal. |
| Citrato urinario | Esperar resultado o medir si no se procesa | Hipocitraturia es factor de riesgo clave para litiasis; su corrección (citrato de potasio) puede ser necesaria. |
| Hidratación | Mantener >2–2.5 L diuresis/día | Disminuye sobresaturación de urato, calcio y fosfato. |
| Dieta | - Reducir carnes rojas, vísceras, mariscos, fructosa- Limitar bebidas cola/ultraprocesados ricos en fosfato | Disminuye urato y fosfato urinarios; ayuda a bajar proteinuria. |
| Peso y ejercicio | Mantener masa muscular adecuada; evitar ejercicio intenso inmediatamente antes de la recolección | Minimiza picos de proteinuria y creatinina. |
| Descartar enfermedades metabólicas | Glicemia, perfil lipídico, ácido úrico sérico, tests de resistencia a insulina | Hiperuricosuria frecuente en síndrome metabólico. |
Aviso: Esta interpretación es educativa y no sustituye la valoración personalizada de un profesional de la salud que conozca su historia clínica completa, medicación y objetivos terapéuticos. Lleve el informe y estas observaciones a su médico para una discusión dirigida.
My A1c is 4.5, blood presión normally Around 125/74 . But yesterday in nephrologist was l150/80. Proteín intake 220g. But since last two weeks i decreased. I feel really frustrated because every doctors ive gone ( two internals and two nephrologist ) didnt find link between my symtpons and test. But i feel really tired and if try to do some exercise i feel really echa usted. I feel lot of pain in flancs too@Goddar What's your A1c, blood pressure, and your protein intake?
Nelson Vergel
Founder, ExcelMale.com
Have them test this:My A1c is 4.5, blood presión normally Around 125/74 . But yesterday in nephrologist was l150/80. Proteín intake 220g. But since last two weeks i decreased. I feel really frustrated because every doctors ive gone ( two internals and two nephrologist ) didnt find link between my symtpons and test. But i feel really tired and if try to do some exercise i feel really echa usted. I feel lot of pain in flancs too

CPK Blood Test (Creatine Phosphokinase) | Discounted Labs
Learn more about the CPK lab test and its significance in diagnosing various health conditions. Buy your own CPK lab test without a doctor visit on DiscountedLabs
Please remind me what medications you are taking.
Not now, next monday.Have them test this:

CPK Blood Test (Creatine Phosphokinase) | Discounted Labs
Learn more about the CPK lab test and its significance in diagnosing various health conditions. Buy your own CPK lab test without a doctor visit on DiscountedLabs
Please remind me what medications you are taking.
I was on 15mg test cyp daily. I discontinued 3 days ago because i read it could affect the tubular.
Pd: i didnt know you are from Venezuela. I love the people of this country
Nelson Vergel
Founder, ExcelMale.com
Thanks. Yes, proud to be Venezuelan and a US citizen. Where do you live ? I noticed your lab test results are in Spanish.Not now, next monday.
I was on 15mg test cyp daily. I discontinued 3 days ago because i read it could affect the tubular.
Pd: i didnt know you are from Venezuela. I love the people of this country
Which part from Venezuela ? Im from Valencia, SpainThanks. Yes, proud to be Venezuelan and a US citizen. Where do you live ? I noticed your lab test results are in Spanish.
Nelson Vergel
Founder, ExcelMale.com
Maracaibo. I am moving to Porto soon. I have heard great things about Valencia.Which part from Venezuela ? Im from Valencia, Spain
Maracucho! I hope Venezuela come Back again before Chavez to visit. Really nice country with bad leadersMaracaibo. I am moving to Porto soon. I have heard great things about Valencia.
ExcelMale Newsletter Signup
Stay Informed with Our Newsletter
Get the latest men's health insights, expert advice, and community updates delivered to your inbox.
Similar threads
- Replies
- 0
- Views
- 2K
- Replies
- 1
- Views
- 4K
- Replies
- 35
- Views
- 3K
- Replies
- 4
- Views
- 3K
TRT Hormone Predictor
Predict estradiol, DHT, and free testosterone levels based on total testosterone
⚠️ Medical Disclaimer
This tool provides predictions based on statistical models and should NOT replace professional medical advice. Always consult with your healthcare provider before making any changes to your TRT protocol.
ℹ️ Input Parameters
Normal range: 300-1000 ng/dL
Predicted Hormone Levels
Enter your total testosterone value to see predictions
Results will appear here after calculation
Understanding Your Hormones
Estradiol (E2)
A form of estrogen produced from testosterone. Important for bone health, mood, and libido. Too high can cause side effects; too low can affect well-being.
DHT
Dihydrotestosterone is a potent androgen derived from testosterone. Affects hair growth, prostate health, and masculinization effects.
Free Testosterone
The biologically active form of testosterone not bound to proteins. Directly available for cellular uptake and biological effects.
Scientific Reference
Lakshman KM, Kaplan B, Travison TG, Basaria S, Knapp PE, Singh AB, LaValley MP, Mazer NA, Bhasin S. The effects of injected testosterone dose and age on the conversion of testosterone to estradiol and dihydrotestosterone in young and older men. J Clin Endocrinol Metab. 2010 Aug;95(8):3955-64.
DOI: 10.1210/jc.2010-0102 | PMID: 20534765 | PMCID: PMC2913038
Online statistics
- Members online
- 5
- Guests online
- 238
- Total visitors
- 243
Totals may include hidden visitors.
Latest posts
-
Nelson Vergel 's Testosterone plus HCG Protocol
- Latest: Fernando Almaguer
-
High Testosterone Levels: Impact on the Heart
- Latest: Fernando Almaguer
-
-
-
-
Impact of GLP-1 receptor agonists on testosterone levels and men’s health
- Latest: Nelson Vergel
-
Adding Anastrozole, how much should I lower dose?
- Latest: Nelson Vergel