madman
Super Moderator
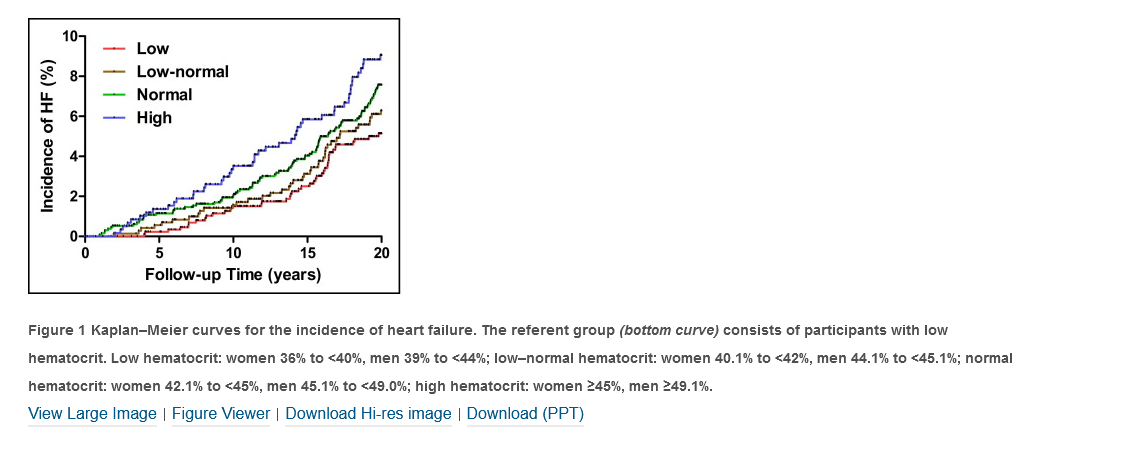
Study Need and Importance: Secondary erythrocytosis, defined as hematocrit (HCt) ≥51% in males, is a well-known consequence of testosterone therapy. Testosterone formulation and route of administration can significantly influence changes in HCt, but the degree of HCt increases has not been compared and quantified across formulations. Head-to-head trials comparing testosterone therapies are rare, meaning that network metaanalysis of contemporary studies is the only way to compare HCt changes by testosterone type. Our study will clarify the magnitude of increases in HCt that have been observed thus far and compare the different effects on HCt between testosterone therapies.
What We Found: We included 29 placebo-controlled randomized trials (3,393 men) to analyze mean HCt change after testosterone therapy by network meta-analysis. All types of testosterone therapies resulted in statistically significant increases in mean HCt when compared with placebo, including gel (3.0%, 95% CI 1.8-4.3), oral testosterone undecanoate (4.3%, 0.7-8.0), patch (1.4%, 0.2-2.6), intramuscular testosterone enanthate/cypionate (4.0%, 2.9-5.1), and intramuscular testosterone undecanoate (1.6%, 0.3-3.0; see figure). When comparing all formulations against one another, intramuscular testosterone cypionate/enanthate was associated with a significantly higher increase in mean HCt compared to patch, but no differences in HCt change between other formulations were detected.
Limitations: This study was limited by the availability and consistency of erythrocytosis event reporting that may have provided us with more clinically significant outcomes, heterogeneity in the inclusion criteria of the trials we selected, and inability to evaluate testosterone pellets or different dosing schedules.
Interpretation for Patient Care: All types of testosterone are associated with increased HCt; however, the clinical concern of this increase remains questionable, warranting future studies. We found that no testosterone therapy formulation had a pooled mean HCt increase over 4.3%, suggesting that the risks of testosterone-induced erythropoiesis may be mitigated through close clinical monitoring and careful patient selection.
Purpose: We sought to compare testosterone formulations and determine the degree that hematocrit increases vary by testosterone therapy formulation. As head-to-head trials are rare, network meta-analysis of the contemporary studies is the only way to compare hematocrit changes by testosterone type, including topical gels and patches, injectables (both short-acting and long-acting), and oral tablets.
Materials and Methods: We conducted a thorough search of listed publications in Scopus, PubMed, Embase, Cochrane CENTRAL, and ClinicalTrials.gov. A total of 29 placebo-controlled randomized trials (3,393 men) met inclusion criteria for analysis of mean hematocrit change after testosterone therapy. Randomized controlled trial data for the following formulations of testosterone were pooled via network meta-analysis: gel, patch, oral testosterone undecanoate, intramuscular testosterone undecanoate, and intramuscular testosterone enanthate/cypionate.
Results: All types of testosterone therapies result in statistically significant increases in mean hematocrit when compared with placebo. Meta-analysis revealed all formulations, including gel (3.0%, 95% CI 1.8-4.3), oral testosterone undecanoate (4.3%, 0.7-8.0), patch (1.4%, 0.2-2.6), intramuscular testosterone enanthate/cypionate (4.0%, 2.9-5.1), and intramuscular testosterone undecanoate (1.6%, 0.3-3.0) result in statistically significant increases in mean hematocrit when compared with placebo. When comparing all formulations against one another, intramuscular testosterone cypionate/enanthate was associated with a significantly higher increase in mean hematocrit compared to patch, but no differences in hematocrit between other formulations were detected.
Conclusions: All types of testosterone are associated with increased hematocrit; however, the clinical concern of this increase remains questionable, warranting future studies. This is the first network meta-analysis to quantify mean hematocrit change and compare formulations, given the absence of head-to-head trials.
TESTOSTERONE deficiency is estimated to affect roughly a quarter of all men,1 with rates set to rise as the population continues to age. This trend, coupled with the positive relationship between testosterone levels and quality of life,2 has likely contributed to the dramatic rise in androgen prescription rates in the 21st century.3 Given these trends in testosterone therapy (TT) prescribing patterns, it is important that we thoroughly investigate any associated risks.4,5 Secondary erythrocytosis, defined as erythrocyte mass that exceeds 125% of predicted6 or >51% in males,7 is one such consequence that has long been associated with TT.8,9 Venous thromboembolism and major adverse cardiac event are the most concerning risks associated with increased hematocrit (HCt),10-13 warranting further investigation into any factor that increases blood viscosity.
Increases of HCt observed with TT are dose-dependent9 and serum-level-dependent.14 The literature currently shows that the varying pharmacokinetics, dosage, and route of administration lead to unique adverse effect profiles for each formulation.15,16 Given these variations in the effects of different TT formulations, we hypothesized that different TT formulations would lead to varying levels of HCt increases. Current literature is lacking in head-to-head randomized controlled trials (RCTs) that compare the effects of different TT formulations, requiring that the network meta-analysis technique be used to evaluate formulations against one another.17 Network meta-analysis is a robust statistical technique for comparing the effects of multiple treatment arms against one another across several compiled studies, and it is the optimal way to compare the effects of different treatments in the absence of head-to-head RCTs.17
Previously, network meta-analysis has been used to describe various differences in TT formulation effects, such as serum testosterone changes, quality of life, and rates of documented erythrocytosis.18 However, there has not yet been a network meta-analysis to quantify the average increase in HCt for each TT formulation, which may be a more reliable measure of the erythropoietic effect of testosterone than documented erythrocytosis due to variations in participant exclusion criteria, the pre-defined cutoff point for “erythrocytosis,” and adverse event reporting across studies.
We conducted a systematic review and network meta-analysis of RCTs controlling against either placebo or standard treatment (active-controlled) that evaluated and compared gel, patch, oral testosterone undecanoate (TU), intramuscular (IM) TU, and IM testosterone enanthate/cypionate (TE/C) formulations against placebo and one another. We emphasized a comprehensive review of the existing literature and employed a rigorous evaluation of study quality in order to ensure reliable estimations of the effects of different TT formulations could be obtained. Our study will clarify the magnitude of increases in HCt that have been observed thus far and compare the different effects on HCt between TT types.
*Compared to similar investigations into the topic, to our knowledge, this study is the first to investigate the effect of different formulations on mean HCt difference through a network meta-analysis. Our findings suggest that while all types of TT should be expected to increase HCt, the risk of pathological erythrocytosis when treating testosterone deficient men in a controlled setting remains relatively low.
.
CONCLUSIONS
All formulations of TT are associated with a mean increase in HCt, but the clinical significance of this increase remains unclear. IM TE/C had a significantly higher change in HCt compared to patch, but there were no significant differences in HCt change between other treatment arms. This is the first study to use network meta-analysis to make comparisons between TT modalities and quantify the mean increase in HCt. Future studies are necessary to assess the actual health risks of TT, including rates of erythrocytosis and whether erythrocytosis will be associated with major adverse cardiovascular events such as venous thromboembolism and mortality.
What We Found: We included 29 placebo-controlled randomized trials (3,393 men) to analyze mean HCt change after testosterone therapy by network meta-analysis. All types of testosterone therapies resulted in statistically significant increases in mean HCt when compared with placebo, including gel (3.0%, 95% CI 1.8-4.3), oral testosterone undecanoate (4.3%, 0.7-8.0), patch (1.4%, 0.2-2.6), intramuscular testosterone enanthate/cypionate (4.0%, 2.9-5.1), and intramuscular testosterone undecanoate (1.6%, 0.3-3.0; see figure). When comparing all formulations against one another, intramuscular testosterone cypionate/enanthate was associated with a significantly higher increase in mean HCt compared to patch, but no differences in HCt change between other formulations were detected.
Limitations: This study was limited by the availability and consistency of erythrocytosis event reporting that may have provided us with more clinically significant outcomes, heterogeneity in the inclusion criteria of the trials we selected, and inability to evaluate testosterone pellets or different dosing schedules.
Interpretation for Patient Care: All types of testosterone are associated with increased HCt; however, the clinical concern of this increase remains questionable, warranting future studies. We found that no testosterone therapy formulation had a pooled mean HCt increase over 4.3%, suggesting that the risks of testosterone-induced erythropoiesis may be mitigated through close clinical monitoring and careful patient selection.
Purpose: We sought to compare testosterone formulations and determine the degree that hematocrit increases vary by testosterone therapy formulation. As head-to-head trials are rare, network meta-analysis of the contemporary studies is the only way to compare hematocrit changes by testosterone type, including topical gels and patches, injectables (both short-acting and long-acting), and oral tablets.
Materials and Methods: We conducted a thorough search of listed publications in Scopus, PubMed, Embase, Cochrane CENTRAL, and ClinicalTrials.gov. A total of 29 placebo-controlled randomized trials (3,393 men) met inclusion criteria for analysis of mean hematocrit change after testosterone therapy. Randomized controlled trial data for the following formulations of testosterone were pooled via network meta-analysis: gel, patch, oral testosterone undecanoate, intramuscular testosterone undecanoate, and intramuscular testosterone enanthate/cypionate.
Results: All types of testosterone therapies result in statistically significant increases in mean hematocrit when compared with placebo. Meta-analysis revealed all formulations, including gel (3.0%, 95% CI 1.8-4.3), oral testosterone undecanoate (4.3%, 0.7-8.0), patch (1.4%, 0.2-2.6), intramuscular testosterone enanthate/cypionate (4.0%, 2.9-5.1), and intramuscular testosterone undecanoate (1.6%, 0.3-3.0) result in statistically significant increases in mean hematocrit when compared with placebo. When comparing all formulations against one another, intramuscular testosterone cypionate/enanthate was associated with a significantly higher increase in mean hematocrit compared to patch, but no differences in hematocrit between other formulations were detected.
Conclusions: All types of testosterone are associated with increased hematocrit; however, the clinical concern of this increase remains questionable, warranting future studies. This is the first network meta-analysis to quantify mean hematocrit change and compare formulations, given the absence of head-to-head trials.
TESTOSTERONE deficiency is estimated to affect roughly a quarter of all men,1 with rates set to rise as the population continues to age. This trend, coupled with the positive relationship between testosterone levels and quality of life,2 has likely contributed to the dramatic rise in androgen prescription rates in the 21st century.3 Given these trends in testosterone therapy (TT) prescribing patterns, it is important that we thoroughly investigate any associated risks.4,5 Secondary erythrocytosis, defined as erythrocyte mass that exceeds 125% of predicted6 or >51% in males,7 is one such consequence that has long been associated with TT.8,9 Venous thromboembolism and major adverse cardiac event are the most concerning risks associated with increased hematocrit (HCt),10-13 warranting further investigation into any factor that increases blood viscosity.
Increases of HCt observed with TT are dose-dependent9 and serum-level-dependent.14 The literature currently shows that the varying pharmacokinetics, dosage, and route of administration lead to unique adverse effect profiles for each formulation.15,16 Given these variations in the effects of different TT formulations, we hypothesized that different TT formulations would lead to varying levels of HCt increases. Current literature is lacking in head-to-head randomized controlled trials (RCTs) that compare the effects of different TT formulations, requiring that the network meta-analysis technique be used to evaluate formulations against one another.17 Network meta-analysis is a robust statistical technique for comparing the effects of multiple treatment arms against one another across several compiled studies, and it is the optimal way to compare the effects of different treatments in the absence of head-to-head RCTs.17
Previously, network meta-analysis has been used to describe various differences in TT formulation effects, such as serum testosterone changes, quality of life, and rates of documented erythrocytosis.18 However, there has not yet been a network meta-analysis to quantify the average increase in HCt for each TT formulation, which may be a more reliable measure of the erythropoietic effect of testosterone than documented erythrocytosis due to variations in participant exclusion criteria, the pre-defined cutoff point for “erythrocytosis,” and adverse event reporting across studies.
We conducted a systematic review and network meta-analysis of RCTs controlling against either placebo or standard treatment (active-controlled) that evaluated and compared gel, patch, oral testosterone undecanoate (TU), intramuscular (IM) TU, and IM testosterone enanthate/cypionate (TE/C) formulations against placebo and one another. We emphasized a comprehensive review of the existing literature and employed a rigorous evaluation of study quality in order to ensure reliable estimations of the effects of different TT formulations could be obtained. Our study will clarify the magnitude of increases in HCt that have been observed thus far and compare the different effects on HCt between TT types.
*Compared to similar investigations into the topic, to our knowledge, this study is the first to investigate the effect of different formulations on mean HCt difference through a network meta-analysis. Our findings suggest that while all types of TT should be expected to increase HCt, the risk of pathological erythrocytosis when treating testosterone deficient men in a controlled setting remains relatively low.
.
CONCLUSIONS
All formulations of TT are associated with a mean increase in HCt, but the clinical significance of this increase remains unclear. IM TE/C had a significantly higher change in HCt compared to patch, but there were no significant differences in HCt change between other treatment arms. This is the first study to use network meta-analysis to make comparisons between TT modalities and quantify the mean increase in HCt. Future studies are necessary to assess the actual health risks of TT, including rates of erythrocytosis and whether erythrocytosis will be associated with major adverse cardiovascular events such as venous thromboembolism and mortality.