BadassBlues
Well-Known Member
The Clinical Potential of Senolytic Drugs
The Clinical Potential of Senolytic Drugs
Senolytic drugs are agents that selectively induce apoptosis of senescent cells. These cells accumulate in many tissues with aging and at sites of pathology in multiple chronic diseases. In studies in animals, targeting senescent cells using genetic or pharmacological approaches delays, prevents, or alleviates multiple age-related phenotypes, chronic diseases, geriatric syndromes, and loss of physiological resilience. Among the chronic conditions successfully treated by depleting senescent cells in preclinical studies are frailty, cardiac dysfunction, vascular hyporeactivity and calcification, diabetes mellitus, liver steatosis, osteoporosis, vertebral disk degeneration, pulmonary fibrosis, and radiation-induced damage. Senolytic agents are being tested in proof-of-concept clinical trials. To do so, new clinical trial paradigms for testing senolytics and other agents that target fundamental aging mechanisms are being developed, because use of long-term endpoints such as lifespan or healthspan is not feasible. These strategies include testing effects on multimorbidity, accelerated aging-like conditions, diseases with localized accumulation of senescent cells, potentially fatal diseases associated with senescent cell accumulation, age-related loss of physiological resilience, and frailty. If senolytics or other interventions that target fundamental aging processes prove to be effective and safe in clinical trials, they could transform geriatric medicine by enabling prevention or treatment of multiple diseases and functional deficits in parallel, instead of one at a time.
Senolytic - Wikipedia
A senolytic (from the words senescence and -lytic, "destroying") is among a class of small molecules under basic research to determine if they can selectively induce death of senescent cells and improve health in humans.[1] A goal of this research is to discover or develop agents to delay, prevent, alleviate, or reverse age-related diseases.[2][3] A related concept is "senostatic", which means to suppress senescence.
USP7 inhibitors | Inhibitors of USP7 (ubiquitin-specific processing protease 7)[15] | Yes[20] | Yes[20] | ||||
SSK1 | Senescence-specific killing compound 1: A gemcitabine (a cytotoxic chemotherapeutic) prodrug that is activated by lysosomal β-galactosidase (a common senescence marker)[27] | Yes[27] | |||||
Src tyrosine kinase inhibitors: dasatinib[19] – see "Combination of dasatinib and quercetin" below | |||||||
Yes[35] | |||||||
Yes[25] | |||||||
xenograft | Yes[24] | ||||||
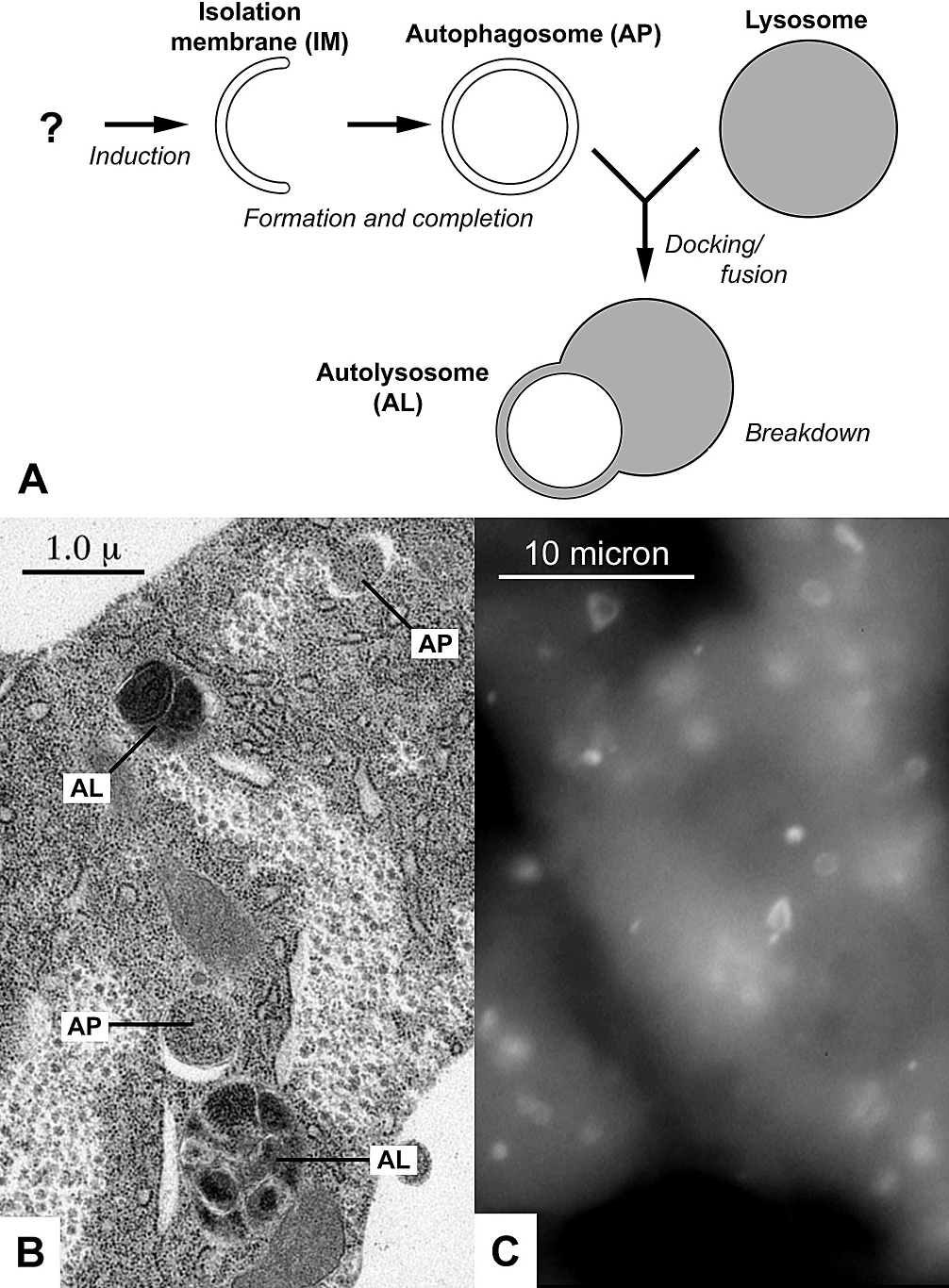
GLS1 inhibitors | Target the enzyme kidney-type glutaminase 1 (GLS1). Senescent cells have a low pH due to their high lysosomal content and leaking lysosomal membranes. This low pH forms the basis of senescence-associated beta-galactosidase (SA-β-gal) staining of senescent cells. To help neutralize their low pH, senescent cells produce high levels of GLS1; inhibiting the activity of this enzyme exposes senescent cells to unsurvivably severe internal acidity, leading to cell death.[29] | Yes[29] | |||||
FOXO4 binding to p53 protein retains it in the nucleus, which prevents it from interacting with mitochondria in the cytosol where it would activate caspases, leading to apoptosis (programmed cell death).[16] Instead, retention of p53 in the nucleus by FOXO4 promotes cellular senescence.[16] A peptide that binds with FOXO4 disrupts the p53-FOXO4 interaction, releasing p53 into the cytosol and triggering cell death.[16] | Yes[16] | Yes[16] | |||||
Yes[23] | Yes[23] | ||||||
Yes | |||||||
Yes | Yes | ||||||
xenograft | Yes[32] | ||||||
BIRC5 knockout | Crispr/Cas9 BIRC5 Gene Knockout. Crispr/Cas9 is used to trigger apoptosis in relation to a specified gene sequence such as a cancer gene sequence or damage marker sequences.[28] | Yes[28] | |||||
BCL-2 inhibitors | Inhibitors of different members of the bcl-2 family of anti-apoptotic proteins.[11][17][18] Studies of cell cultures of senescent human umbilical vein endothelial cells have shown that both fisetin and quercetin induce apoptosis by inhibition of the anti-apoptotic protein Bcl-xL (a bcl-2 family member).[4] | Yes[4] | |||||
Yes[26] | |||||||
Anti-GPNMB vaccine | Glycoprotein nonmetastatic melanoma protein B (GPNMB). A protein that enrich senescent cells studied as molecular target for a senolytic vaccine in mice.[30] | Yes[30] | |||||
25-hydroxycholesterol (25HC)[34] | 25-hydroxycholesterol targets CRYAB in multiple human and mouse cell types | Yes[34] |