madman
Super Moderator
Haematological actions of androgens (2022)
Annabelle M. Warren, Endocrinologist *, Mathis Grossmann, Endocrinologist
In this review, we discuss the effects of androgens on the haemopoietic system, focussing largely on the effects of testosterone on erythropoiesis. Stimulation of erythropoiesis is one of the most consistent effects of testosterone treatment observed in clinical trials. In men with anaemia, this effect can be beneficial. Conversely, erythrocytosis is one of the most common adverse effects of testosterone treatment with a relative risk of 8.14 (95% CI: 1.87-35.40) estimated by a recent meta-analysis of randomised placebo-controlled clinical trials. A reduction in haemoglobin is commonly seen in men receiving androgen deprivation therapy for prostate cancer, and in transwomen receiving gender-affirming therapy to reduce serum testosterone. While mechanisms by which androgens regulate erythropoiesis are not fully understood, it is likely that effects on erythropoietic progenitor cells and erythropoietin are involved, with secondary effects on iron metabolism. In contrast, whether androgens exert clinically relevant effects on white blood cells and on platelets requires further study.
Introduction
The effects of androgens on the haematological system, particularly erythropoiesis, have long been recognised. It has been observed that men have higher average haemoglobin concentrations than women and that anaemia or even pancytopenia may be seen in men with hypogonadism [1,2]. Prior to the availability of recombinant haematopoietic growth factors, androgens were used as a treatment for anaemia [3]. Current therapeutic uses of androgens in male hypogonadism and gender-affirming hormone therapy in transgender men, as well as androgen abuse for recreational and athletic performance enhancement, provide clinical in vivo models for this effect. On the one hand, testosterone treatment can improve otherwise unexplained anaemia, a therapeutic benefit. On the other hand, testosterone treatment can carry a risk of erythrocytosis (haematocrit > 54%) and related thromboembolic complications. The mechanisms underlying androgen stimulation of red cell production are incompletely understood but are thought to occur through stimulation of erythropoietin (EPO) production and probably direct effects on haematopoietic stem cells, with additional effects on iron regulation such as raised erythroferrone and reduced hepcidin to increase iron availability. The impacts on white cells and platelets are less well described. While a subtle rise in white cell count (particularly neutrophils and monocytes) and platelets has been seen in response to androgens in some studies, the clinical significance of this is less evident.
Red cells and androgens
Differences in haemoglobin concentrations observed between the sexes first provided a clue to the stimulatory effect of androgens on erythropoiesis. A causative relationship between testosterone and red blood cell indices was established in preclinical studies in the 1940s that demonstrated a marked decrease in erythropoiesis after castration of male rats, which could be reversed with the administration of exogenous androgens [4]. Indeed, prior to the availability of recombinant erythropoietin (EPO) in the 1980s, androgens were used clinically as a treatment for anaemia.
There are a variety of clinical scenarios that illustrate the effect of the addition or depletion of both endogenous and exogenous androgens on erythropoiesis. These instructive models have enhanced our understanding of physiology, though it remains incompletely understood.
*Sex differences as a model for androgen effects
*Androgen deficiency and anaemia
*Organic hypogonadism
*Androgen deprivation therapy (ADT)
*Men with age-related decline in serum testosterone
*Androgen therapy and erythrocytosis
‘Erythrocytosis’ is formally defined as a haematocrit 25% higher than expected for an individual's height and weight [39]. The term ‘polycythaemia’ is often used interchangeably, but refers to any haematological cell excess rather than erythrocytes specifically. Erythrocytosis is suspected when haemoglobin is above 185 g/L or the haematocrit greater than 52% in a man, or above 165 g/L and 48% respectively, in a woman [40]. In men on testosterone therapy, the Endocrine society defines erythrocytosis as haematocrit greater than 54%.
Given that testosterone improves anaemia, it is not surprising that erythrocytosis is a recognised complication of testosterone therapy. Prior to the availability of recombinant erythropoietin (EPO), this stimulatory effect of androgens was harnessed to treat renal anaemia, anaemia of chronic disease, aplastic anaemia and the myelodysplastic syndrome [1,3,6]. Indeed, in older patients with aplastic anaemia unsuitable for aggressive immunosuppression, androgens such as danazol or oxymetholone remain in use [41].
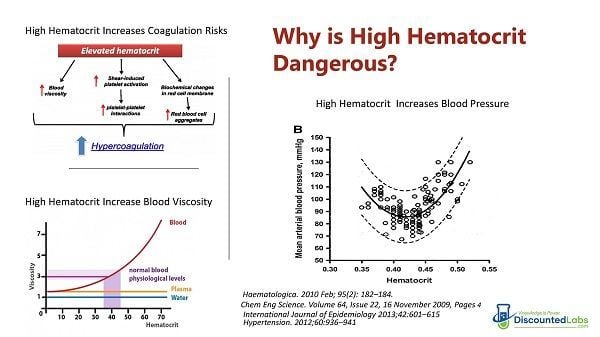
Testosterone treatment-associated erythrocytosis is a potentially significant adverse effect as raised haematocrit is associated with venous thromboembolism, cardiovascular disease and stroke in men with and without underlying hypogonadism [42,43]. However, to date, no randomised clinical trial has shown that testosterone-related increases in haematocrit are associated with increased clinical arterial or venous thrombotic events.
*Testosterone for hypogonadism
A meta-analysis of 19 randomised placebo-controlled trials including 651 testosterone-treated men found that erythrocytosis (defined as an increase in haematocrit over 50%) was the most frequently reported adverse event [44]. Testosterone-treated men were almost four times more likely than placebo-treated men to develop haematocrit >50% (OR 3.96, 95% CI: 1.82e7.51), with an event rate of 64.5 per 1000 patient-years. Reassuringly though, there was no difference in rates of cardiovascular events or death in this moderate sample. Likewise in a more recent meta-analysis of RCTs restricted to men with hypogonadism (defined as at least one symptom or sign of hypogonadism and serum testosterone of <10.4 nmol/L (<300 ng/dL), n = 1579) the most frequent adverse effect associated with testosterone treatment was an increased risk of erythrocytosis (defined as haematocrit >54% or haemoglobin >17.5 g/ dL) (relative risk: 8.14, 95% CI: 1.87-35.40) [45]. The risk of erythrocytosis is dose-related, as reported in a randomised trial of 121 healthy men treated with androgen deprivation and graded exogenous testosterone add-back (5 doses of intramuscular testosterone enanthate 25-600 mg IM weekly) which showed a linear relationship between testosterone dose and increasing haematocrit (r = 0.63,p < 0.0001) [46]. This study also compared the impact of patient age and found higher rates of testosterone-induced erythrocytosis were observed in older men compared with younger men (p < 0.0001). The mechanisms by which older age renders men more susceptible to the pro-erythropoietic actions of testosterone are not understood. While in the aforementioned study [46], older men had higher treatment circulating testosterone concentrations compared to younger men randomized to equivalent testosterone treatment doses, the age effect on haematocrit persisted even after adjustment for these differences in treatment serum testosterone concentrations. Moreover, the age effect was not explained by changes in erythropoietin and soluble transferrin receptor concentrations. It is possible that this increased susceptibility in older men is contributed to by the fact that they are more likely to accumulate age-related comorbidities such as sleep apnoea (see T4DM study below), hypoxic lung disease and overweight/obesity that in turn could predispose them to a heightened sensitivity to the erythropoietic actions of testosterone treatment. It may also relate to the fact that baseline testosterone concentrations decline with age overall, so achieving a standard therapeutic concentration may represent a relatively higher increase in androgen activity
While all testosterone formulations have been associated with an increase in haematocrit, no study has compared the effect of different formulations prospectively in a head-to-head design. In a recent meta-analysis of 29 RCTs (3393 men) comparing different testosterone formulations against one another, intramuscular testosterone esters were associated with a significantly higher increase in haematocrit compared to topical testosterone patch, but no difference in haematocrit between other formulations was detected [47]. A relatively new mode of testosterone treatment is subcutaneous administration. The incidences of erythrocytosis with subcutaneous administration may be higher in transdermal testosterone, although experience with subcutaneous testosterone to date is relatively limited [48]. In contrast, intranasal testosterone may have a lower risk of erythrocytosis [49].
US Endocrine Society guidelines on testosterone therapy in men with hypogonadism recommend careful monitoring of haematocrit and haemoglobin [50]. Therapy should aim for a testosterone concentration within the mid-normal male reference range, as erythrocytosis risk is dose-dependent. If haematocrit does rise above 54% during testosterone replacement, current guidelines advise that therapy should be withheld until the haematocrit has returned to the normal range [50]. It is useful to evaluate for additional contributors such as obstructive sleep apnoea (which causes chronic hypoxia which may also stimulate erythropoiesis). Therapeutic options to allow the continuation of testosterone include smoking cessation, testosterone dose reduction or venesection to lower haematocrit.
*Supplemental testosterone without hypogonadism
*Testosterone for gender-affirming hormone therapy
*Androgen abuse
*Mechanisms of androgen stimulation of erythropoiesis
It has been recognised for many decades that exposure to testosterone increases the number of erythroid colonies in bone marrow culture. The exact mechanism underlying androgenic stimulation of erythropoiesis is incompletely understood, but there is evidence for stimulation of renal erythropoietin (EPO) production, and potentially a direct effect on haemopoietic stem cells to promote erythropoiesis [6]. Further mechanisms involving iron regulatory pathways such as hepcidin and erythroferrone have been explored, however, these may, at least in part, be secondary effects of erythropoiesis stimulation to enhance iron availability, rather than primary mechanisms. The current understanding of the mechanisms is summarised in Fig. 1.
Of note, while some biological actions of testosterone (e.g. on bone and fat mass) are dependent on its aromatisation to estradiol, it is generally accepted that estradiol plays no significant role in mediating the effects of testosterone on erythropoiesis. Indeed, erythrocytosis is a common side effect of non-aromatisable androgens (especially in the context of anabolic steroid abuse), and non-aromatisable DHT has been reported to stimulate haematopoiesis in rodent studies [58]. Moreover, a study in two aromatase-deficient men reported increased erythropoiesis following exposure to testosterone but not oestradiol [59]. Several trials using testosterone treatment in men have reported that the erythropoietic actions of testosterone are not altered by co-treatment with a 5a-reductase inhibitor, implying that conversion of testosterone to DHT is not required for the erythropoietic actions of testosterone [60,61].
*Effects on erythroid progenitor cells
*Erythropoietin
*Hepcidin, erythroferrone and iron availability
Effects of androgens on haemopoietic lineages other than red blood cells
In contrast to the well-established roles of androgens in erythropoiesis, whether androgens exert clinically relevant effects on other haematopoietic lineages is much less well established. There is a wealth of data from pre-clinical models ranging from cell lines to genetically modified animals, such as mice with targeted deletions of the androgen receptor (AR). However, the applicability of the at times very complex findings in preclinical studies to humans is uncertain. Studies using rodents with deletion of the AR do not differentiate developmental effects from those occurring in adults (unless a conditional knockout model is used). Moreover, such studies do not distinguish whether the observed phenotype is due to absent androgen signalling or due to the deletion of the AR itself. Indeed, in mice, haematological phenotypes reported in castration models can differ markedly from those reported in AR knock-out mice (for review, see [31]). Therefore, in the next section, we predominantly discuss findings in humans, noting that only relatively few data from humans are available.
*Androgens and leukocytes
*Androgens and platelets
Summary
Androgens are well established to stimulate erythrocyte production. This relationship manifests clinically as an increased incidence of anaemia in untreated hypogonadal men and those with prostate cancer undergoing androgen deprivation therapy. Conversely, there is a risk of erythrocytosis with testosterone therapy, even when targeting replacement in the cisgender-male reference range, for indications including male hypogonadism and gender affirmation. This risk is dose-dependent, and higher rates of erythrocytosis are seen with supraphysiologic androgen supplementation, including in recreational androgen abuse. Rates of adverse outcomes such as thrombosis from a raised haematocrit are unclear.
The physiology underlying this erythropoietic effect is not fully understood. Androgens increase EPO production via stimulation of renal fibroblast androgen receptors to promote red cell formation, and may also have a direct stimulatory effect on erythroid stem cells in bone marrow beyond EPO enhancement. Changes in iron metabolism observed with androgen therapy, including raised erythroferrone and decreased hepcidin, may at least in part occur as a secondary response to increased red cell production, to increase iron availability to facilitate this process.
The impact of androgens on other haematological cell lines is less understood. Testosterone therapy has been observed to raise neutrophil and monocyte counts, though the clinical implications of this are unclear as androgen deficiency has generally not been reported to cause clinically obvious immunocompromise. Platelet counts may be mildly raised by androgens, and there may be an effect on platelet function with increased expression of the thromboxane-A2 receptor, which may promote platelet aggregation. Further research to understand the mechanisms of androgens' impacts on the haematological system, and better information regarding the implications of erythrocytosis and potentially enhanced platelet aggregation with respect to cardiovascular risk, is awaited.
Annabelle M. Warren, Endocrinologist *, Mathis Grossmann, Endocrinologist
In this review, we discuss the effects of androgens on the haemopoietic system, focussing largely on the effects of testosterone on erythropoiesis. Stimulation of erythropoiesis is one of the most consistent effects of testosterone treatment observed in clinical trials. In men with anaemia, this effect can be beneficial. Conversely, erythrocytosis is one of the most common adverse effects of testosterone treatment with a relative risk of 8.14 (95% CI: 1.87-35.40) estimated by a recent meta-analysis of randomised placebo-controlled clinical trials. A reduction in haemoglobin is commonly seen in men receiving androgen deprivation therapy for prostate cancer, and in transwomen receiving gender-affirming therapy to reduce serum testosterone. While mechanisms by which androgens regulate erythropoiesis are not fully understood, it is likely that effects on erythropoietic progenitor cells and erythropoietin are involved, with secondary effects on iron metabolism. In contrast, whether androgens exert clinically relevant effects on white blood cells and on platelets requires further study.
Introduction
The effects of androgens on the haematological system, particularly erythropoiesis, have long been recognised. It has been observed that men have higher average haemoglobin concentrations than women and that anaemia or even pancytopenia may be seen in men with hypogonadism [1,2]. Prior to the availability of recombinant haematopoietic growth factors, androgens were used as a treatment for anaemia [3]. Current therapeutic uses of androgens in male hypogonadism and gender-affirming hormone therapy in transgender men, as well as androgen abuse for recreational and athletic performance enhancement, provide clinical in vivo models for this effect. On the one hand, testosterone treatment can improve otherwise unexplained anaemia, a therapeutic benefit. On the other hand, testosterone treatment can carry a risk of erythrocytosis (haematocrit > 54%) and related thromboembolic complications. The mechanisms underlying androgen stimulation of red cell production are incompletely understood but are thought to occur through stimulation of erythropoietin (EPO) production and probably direct effects on haematopoietic stem cells, with additional effects on iron regulation such as raised erythroferrone and reduced hepcidin to increase iron availability. The impacts on white cells and platelets are less well described. While a subtle rise in white cell count (particularly neutrophils and monocytes) and platelets has been seen in response to androgens in some studies, the clinical significance of this is less evident.
Red cells and androgens
Differences in haemoglobin concentrations observed between the sexes first provided a clue to the stimulatory effect of androgens on erythropoiesis. A causative relationship between testosterone and red blood cell indices was established in preclinical studies in the 1940s that demonstrated a marked decrease in erythropoiesis after castration of male rats, which could be reversed with the administration of exogenous androgens [4]. Indeed, prior to the availability of recombinant erythropoietin (EPO) in the 1980s, androgens were used clinically as a treatment for anaemia.
There are a variety of clinical scenarios that illustrate the effect of the addition or depletion of both endogenous and exogenous androgens on erythropoiesis. These instructive models have enhanced our understanding of physiology, though it remains incompletely understood.
*Sex differences as a model for androgen effects
*Androgen deficiency and anaemia
*Organic hypogonadism
*Androgen deprivation therapy (ADT)
*Men with age-related decline in serum testosterone
*Androgen therapy and erythrocytosis
‘Erythrocytosis’ is formally defined as a haematocrit 25% higher than expected for an individual's height and weight [39]. The term ‘polycythaemia’ is often used interchangeably, but refers to any haematological cell excess rather than erythrocytes specifically. Erythrocytosis is suspected when haemoglobin is above 185 g/L or the haematocrit greater than 52% in a man, or above 165 g/L and 48% respectively, in a woman [40]. In men on testosterone therapy, the Endocrine society defines erythrocytosis as haematocrit greater than 54%.
Given that testosterone improves anaemia, it is not surprising that erythrocytosis is a recognised complication of testosterone therapy. Prior to the availability of recombinant erythropoietin (EPO), this stimulatory effect of androgens was harnessed to treat renal anaemia, anaemia of chronic disease, aplastic anaemia and the myelodysplastic syndrome [1,3,6]. Indeed, in older patients with aplastic anaemia unsuitable for aggressive immunosuppression, androgens such as danazol or oxymetholone remain in use [41].
Testosterone treatment-associated erythrocytosis is a potentially significant adverse effect as raised haematocrit is associated with venous thromboembolism, cardiovascular disease and stroke in men with and without underlying hypogonadism [42,43]. However, to date, no randomised clinical trial has shown that testosterone-related increases in haematocrit are associated with increased clinical arterial or venous thrombotic events.
*Testosterone for hypogonadism
A meta-analysis of 19 randomised placebo-controlled trials including 651 testosterone-treated men found that erythrocytosis (defined as an increase in haematocrit over 50%) was the most frequently reported adverse event [44]. Testosterone-treated men were almost four times more likely than placebo-treated men to develop haematocrit >50% (OR 3.96, 95% CI: 1.82e7.51), with an event rate of 64.5 per 1000 patient-years. Reassuringly though, there was no difference in rates of cardiovascular events or death in this moderate sample. Likewise in a more recent meta-analysis of RCTs restricted to men with hypogonadism (defined as at least one symptom or sign of hypogonadism and serum testosterone of <10.4 nmol/L (<300 ng/dL), n = 1579) the most frequent adverse effect associated with testosterone treatment was an increased risk of erythrocytosis (defined as haematocrit >54% or haemoglobin >17.5 g/ dL) (relative risk: 8.14, 95% CI: 1.87-35.40) [45]. The risk of erythrocytosis is dose-related, as reported in a randomised trial of 121 healthy men treated with androgen deprivation and graded exogenous testosterone add-back (5 doses of intramuscular testosterone enanthate 25-600 mg IM weekly) which showed a linear relationship between testosterone dose and increasing haematocrit (r = 0.63,p < 0.0001) [46]. This study also compared the impact of patient age and found higher rates of testosterone-induced erythrocytosis were observed in older men compared with younger men (p < 0.0001). The mechanisms by which older age renders men more susceptible to the pro-erythropoietic actions of testosterone are not understood. While in the aforementioned study [46], older men had higher treatment circulating testosterone concentrations compared to younger men randomized to equivalent testosterone treatment doses, the age effect on haematocrit persisted even after adjustment for these differences in treatment serum testosterone concentrations. Moreover, the age effect was not explained by changes in erythropoietin and soluble transferrin receptor concentrations. It is possible that this increased susceptibility in older men is contributed to by the fact that they are more likely to accumulate age-related comorbidities such as sleep apnoea (see T4DM study below), hypoxic lung disease and overweight/obesity that in turn could predispose them to a heightened sensitivity to the erythropoietic actions of testosterone treatment. It may also relate to the fact that baseline testosterone concentrations decline with age overall, so achieving a standard therapeutic concentration may represent a relatively higher increase in androgen activity
While all testosterone formulations have been associated with an increase in haematocrit, no study has compared the effect of different formulations prospectively in a head-to-head design. In a recent meta-analysis of 29 RCTs (3393 men) comparing different testosterone formulations against one another, intramuscular testosterone esters were associated with a significantly higher increase in haematocrit compared to topical testosterone patch, but no difference in haematocrit between other formulations was detected [47]. A relatively new mode of testosterone treatment is subcutaneous administration. The incidences of erythrocytosis with subcutaneous administration may be higher in transdermal testosterone, although experience with subcutaneous testosterone to date is relatively limited [48]. In contrast, intranasal testosterone may have a lower risk of erythrocytosis [49].
US Endocrine Society guidelines on testosterone therapy in men with hypogonadism recommend careful monitoring of haematocrit and haemoglobin [50]. Therapy should aim for a testosterone concentration within the mid-normal male reference range, as erythrocytosis risk is dose-dependent. If haematocrit does rise above 54% during testosterone replacement, current guidelines advise that therapy should be withheld until the haematocrit has returned to the normal range [50]. It is useful to evaluate for additional contributors such as obstructive sleep apnoea (which causes chronic hypoxia which may also stimulate erythropoiesis). Therapeutic options to allow the continuation of testosterone include smoking cessation, testosterone dose reduction or venesection to lower haematocrit.
*Supplemental testosterone without hypogonadism
*Testosterone for gender-affirming hormone therapy
*Androgen abuse
*Mechanisms of androgen stimulation of erythropoiesis
It has been recognised for many decades that exposure to testosterone increases the number of erythroid colonies in bone marrow culture. The exact mechanism underlying androgenic stimulation of erythropoiesis is incompletely understood, but there is evidence for stimulation of renal erythropoietin (EPO) production, and potentially a direct effect on haemopoietic stem cells to promote erythropoiesis [6]. Further mechanisms involving iron regulatory pathways such as hepcidin and erythroferrone have been explored, however, these may, at least in part, be secondary effects of erythropoiesis stimulation to enhance iron availability, rather than primary mechanisms. The current understanding of the mechanisms is summarised in Fig. 1.
Of note, while some biological actions of testosterone (e.g. on bone and fat mass) are dependent on its aromatisation to estradiol, it is generally accepted that estradiol plays no significant role in mediating the effects of testosterone on erythropoiesis. Indeed, erythrocytosis is a common side effect of non-aromatisable androgens (especially in the context of anabolic steroid abuse), and non-aromatisable DHT has been reported to stimulate haematopoiesis in rodent studies [58]. Moreover, a study in two aromatase-deficient men reported increased erythropoiesis following exposure to testosterone but not oestradiol [59]. Several trials using testosterone treatment in men have reported that the erythropoietic actions of testosterone are not altered by co-treatment with a 5a-reductase inhibitor, implying that conversion of testosterone to DHT is not required for the erythropoietic actions of testosterone [60,61].
*Effects on erythroid progenitor cells
*Erythropoietin
*Hepcidin, erythroferrone and iron availability
Effects of androgens on haemopoietic lineages other than red blood cells
In contrast to the well-established roles of androgens in erythropoiesis, whether androgens exert clinically relevant effects on other haematopoietic lineages is much less well established. There is a wealth of data from pre-clinical models ranging from cell lines to genetically modified animals, such as mice with targeted deletions of the androgen receptor (AR). However, the applicability of the at times very complex findings in preclinical studies to humans is uncertain. Studies using rodents with deletion of the AR do not differentiate developmental effects from those occurring in adults (unless a conditional knockout model is used). Moreover, such studies do not distinguish whether the observed phenotype is due to absent androgen signalling or due to the deletion of the AR itself. Indeed, in mice, haematological phenotypes reported in castration models can differ markedly from those reported in AR knock-out mice (for review, see [31]). Therefore, in the next section, we predominantly discuss findings in humans, noting that only relatively few data from humans are available.
*Androgens and leukocytes
*Androgens and platelets
Summary
Androgens are well established to stimulate erythrocyte production. This relationship manifests clinically as an increased incidence of anaemia in untreated hypogonadal men and those with prostate cancer undergoing androgen deprivation therapy. Conversely, there is a risk of erythrocytosis with testosterone therapy, even when targeting replacement in the cisgender-male reference range, for indications including male hypogonadism and gender affirmation. This risk is dose-dependent, and higher rates of erythrocytosis are seen with supraphysiologic androgen supplementation, including in recreational androgen abuse. Rates of adverse outcomes such as thrombosis from a raised haematocrit are unclear.
The physiology underlying this erythropoietic effect is not fully understood. Androgens increase EPO production via stimulation of renal fibroblast androgen receptors to promote red cell formation, and may also have a direct stimulatory effect on erythroid stem cells in bone marrow beyond EPO enhancement. Changes in iron metabolism observed with androgen therapy, including raised erythroferrone and decreased hepcidin, may at least in part occur as a secondary response to increased red cell production, to increase iron availability to facilitate this process.
The impact of androgens on other haematological cell lines is less understood. Testosterone therapy has been observed to raise neutrophil and monocyte counts, though the clinical implications of this are unclear as androgen deficiency has generally not been reported to cause clinically obvious immunocompromise. Platelet counts may be mildly raised by androgens, and there may be an effect on platelet function with increased expression of the thromboxane-A2 receptor, which may promote platelet aggregation. Further research to understand the mechanisms of androgens' impacts on the haematological system, and better information regarding the implications of erythrocytosis and potentially enhanced platelet aggregation with respect to cardiovascular risk, is awaited.