You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Dr Saya Presents a Case Study for Possible Upper Limit of Physiologic Estradiol Levels in a Male
- Thread starter Dr Justin Saya MD
- Start date
Dr Justin Saya MD
Moderator
Formatting wouldn't cooperate with pasting plain text...hopefully everyone can open attachment (or mods can paste plain text). Enjoy!
Vince Carter
Banned
Case Study: Observations of Testosterone/Estradiol Levels and HPTA Response in a MTF Transgender Patient Undergoing Hormonal Feminization Therapy
Dr Justin Saya, MD Defy Medical May 11, 2016
Case Presentation
Patient consent was obtained to use laboratory data and case details from patient, however care is taken to maintain patient privacy and limit any potentially identifying information.
Patient is a biological male presenting at an age of 20 – 25 years old having been referred by his counselor for hormonal treatment to assist MTF transgender transformation. A thorough examination and consult was performed on patient including counseling, lab review, and all appropriate consents were reviewed and signed. Once appropriateness of treatment was determined, MTF transformative hormonal treatment was initiated in the form of estradiol cypionate twice weekly injections. For the purpose of simplicity and a focused discussion, dosages of estradiol cypionate will not be included, but rather the resulting serum estradiol levels (via LC-MS/MS) from gradual estradiol cypionate dosage escalation.
Results/Data
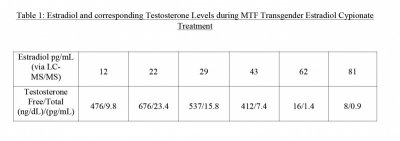
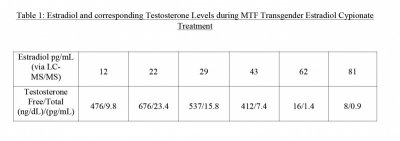
Estradiol (pg/mL) and total/free testosterone (ng/dL – pg/mL) levels were monitored for this patient with the results throughout the first year of treatment documented below in Table 1. Note, as estradiol cypionate dosages were gradually increased over the course of the year (left to right), estradiol lab values via LC-MS/MS increased as expected. There was also an interesting pattern that emerged in the concurrent serum testosterone levels which will be discussed below.
Discussion/Conclusions
It is a well-documented physiologic phenomenon that the endocrine system operates under the principle of “negative feedback”, whereby end-product hormones (i.e. testosterone, estradiol, etc) exert suppression via a negative feedback loop to the hypothalamus – pituitary. This negative feedback loop operates primarily as an evolutionary safety/preventative mechanism to maintain physiologic hormone levels and prevent artificially high or “supra-physiologic” hormone levels (and the resulting health/survival risks attributed to same). Of course, this negative feedback loop can be “over-ridden” through the administration of exogenous hormones (estradiol cypionate, testosterone cypionate, etc), thereby allowing one to achieve supra-physiologic hormone levels without the limitations imposed by negative feedback.
In other words, being able to increase hormone levels (T, E, etc) above the biological “set point” or “limit point” where negative feedback kicks in to prevent further escalation. I would also argue, as a scientist/physician, that determining where this “set point” or “limit point” is would offer insight into determining where various hormone levels are intended to be by biological design. After all, who could argue against the wisdom of our biological design/blueprint?
Evaluating this data reveals an interesting pattern. It was observed that as estradiol cypionate treatment was initiated and resultant estradiol serum levels increased, there was initially an increase in testosterone levels above baseline values. This pattern was observed as estradiol levels increased from 12 pg/mL ->
22pg/mL -> 29pg/mL (with corresponding T levels 476/9.8 -> 676/23.4 -> 537/15.8). Clearly there was NO HPTA suppression as estradiol levels increased from 12pg/mL to 29pg/mL, arguably indicating that these estradiol levels are within the design of biological physiologic levels. In fact, as testosterone levels actually INCREASED as estradiol levels increased from 12pg/mL -> 22pg/mL it may be argued that there was HPTA STIMULATION achieved from this increase in estradiol from 12->22 and, consequently, estradiol levels of 22pg/mL are biologically preferred (or “encouraged/supported” by the HPT axis). This would actually fit nicely with most prevailing current data that estradiol levels below 20pg/mL may
impart certain health risks (interesting isn't it).
Equally as interesting was the pattern that emerged as estradiol levels continued to climb. From the data it appears HPTA suppression began to exert its impact as estradiol levels climbed to 43pg/mL. Note, although LH/FSH levels were not measured in this case as a measurement of HPTA suppression, the decline in T levels as E levels increase (only attributable to HPTA suppression from exogenous E treatment) is used as an indicator for PRESUMPTIVE HPTA suppression. As estradiol levels reached
43pg/mL it appears the HPTA suppression was beginning as this was the first time that testosterone levels were suppressed to below initial baseline levels (476/9.8 baseline vs 412/7.4). Upon further analysis of the data, it is also clear that as estradiol levels continued to climb from 43->62 ->81, there was a profound and powerful HPTA suppression (via negative feedback from increasing estradiol levels) that kicked in to drastically suppress testosterone levels 412/7.4 -> 16/1.4 -> 8/0.9. Thus, in summary, it appears that for this particular biologically male patient, mild HPTA suppression was beginning to exert negative feedback effects as estradiol levels rose to 43pg/mL and this HPTA suppression via negative feedback accelerated rapidly to almost complete suppression by the time estradiol levels had increased to
62pg/mL.
So what does this mean? Perhaps nothing, or perhaps this may point to a "biological set point" or "biological upper limit/ceiling" for estradiol levels in genetic males, after which profound HPTA suppression kicks in as a preventative/protective measure to prevent further increase. If this is the case, it would appear this “ceiling” or biological upper set-point for estradiol (when exposed to normal physiologic endocrine feedback mechanisms) would lie somewhere in the range of 43pg/mL – 62 pg/mL. However, with the HPTA suppression appearing to begin with estradiol levels in the 40's and the drastic/profound suppression evident with estradiol levels of 62 pg/mL, I would argue that the “set- point” or “biological ceiling” would seem to be somewhere between these two extremes, with an educated assumption based on these data and my own clinical experience of 50-55pg/mL. Further, it would be a sound argument to state that any estradiol levels that fall outside (above) the biological set point (wherever that may be) for HPTA suppression (which once again is ingrained into our endocrine system as a self-limiting protective mechanism) would classify as supra-physiologic (i.e. above the levels for which normal HPTA suppression in a male would PREVENT levels from rising).
There are limitations to this study including small sample size, not monitoring LH/FSH but instead relying on observed testosterone suppression as a surrogate measure of HPTA suppression, and lack of more precise measurement of estradiol levels, particularly during the interval of apparent HPTA suppression of 43pg/mL – 62pg/mL. Nonetheless, I feel that this data represents a unique and novel insight into what one might consider ‘physiologic” estradiol levels as measured by the endocrine system's own measuring stick – HPTA suppression via the evolutionary negative feedback mechanism.
Dr Justin Saya, MD Defy Medical May 11, 2016
Case Presentation
Patient consent was obtained to use laboratory data and case details from patient, however care is taken to maintain patient privacy and limit any potentially identifying information.
Patient is a biological male presenting at an age of 20 – 25 years old having been referred by his counselor for hormonal treatment to assist MTF transgender transformation. A thorough examination and consult was performed on patient including counseling, lab review, and all appropriate consents were reviewed and signed. Once appropriateness of treatment was determined, MTF transformative hormonal treatment was initiated in the form of estradiol cypionate twice weekly injections. For the purpose of simplicity and a focused discussion, dosages of estradiol cypionate will not be included, but rather the resulting serum estradiol levels (via LC-MS/MS) from gradual estradiol cypionate dosage escalation.
Results/Data
Estradiol (pg/mL) and total/free testosterone (ng/dL – pg/mL) levels were monitored for this patient with the results throughout the first year of treatment documented below in Table 1. Note, as estradiol cypionate dosages were gradually increased over the course of the year (left to right), estradiol lab values via LC-MS/MS increased as expected. There was also an interesting pattern that emerged in the concurrent serum testosterone levels which will be discussed below.
Discussion/Conclusions
It is a well-documented physiologic phenomenon that the endocrine system operates under the principle of “negative feedback”, whereby end-product hormones (i.e. testosterone, estradiol, etc) exert suppression via a negative feedback loop to the hypothalamus – pituitary. This negative feedback loop operates primarily as an evolutionary safety/preventative mechanism to maintain physiologic hormone levels and prevent artificially high or “supra-physiologic” hormone levels (and the resulting health/survival risks attributed to same). Of course, this negative feedback loop can be “over-ridden” through the administration of exogenous hormones (estradiol cypionate, testosterone cypionate, etc), thereby allowing one to achieve supra-physiologic hormone levels without the limitations imposed by negative feedback.
In other words, being able to increase hormone levels (T, E, etc) above the biological “set point” or “limit point” where negative feedback kicks in to prevent further escalation. I would also argue, as a scientist/physician, that determining where this “set point” or “limit point” is would offer insight into determining where various hormone levels are intended to be by biological design. After all, who could argue against the wisdom of our biological design/blueprint?
Evaluating this data reveals an interesting pattern. It was observed that as estradiol cypionate treatment was initiated and resultant estradiol serum levels increased, there was initially an increase in testosterone levels above baseline values. This pattern was observed as estradiol levels increased from 12 pg/mL ->
22pg/mL -> 29pg/mL (with corresponding T levels 476/9.8 -> 676/23.4 -> 537/15.8). Clearly there was NO HPTA suppression as estradiol levels increased from 12pg/mL to 29pg/mL, arguably indicating that these estradiol levels are within the design of biological physiologic levels. In fact, as testosterone levels actually INCREASED as estradiol levels increased from 12pg/mL -> 22pg/mL it may be argued that there was HPTA STIMULATION achieved from this increase in estradiol from 12->22 and, consequently, estradiol levels of 22pg/mL are biologically preferred (or “encouraged/supported” by the HPT axis). This would actually fit nicely with most prevailing current data that estradiol levels below 20pg/mL may
impart certain health risks (interesting isn't it).
Equally as interesting was the pattern that emerged as estradiol levels continued to climb. From the data it appears HPTA suppression began to exert its impact as estradiol levels climbed to 43pg/mL. Note, although LH/FSH levels were not measured in this case as a measurement of HPTA suppression, the decline in T levels as E levels increase (only attributable to HPTA suppression from exogenous E treatment) is used as an indicator for PRESUMPTIVE HPTA suppression. As estradiol levels reached
43pg/mL it appears the HPTA suppression was beginning as this was the first time that testosterone levels were suppressed to below initial baseline levels (476/9.8 baseline vs 412/7.4). Upon further analysis of the data, it is also clear that as estradiol levels continued to climb from 43->62 ->81, there was a profound and powerful HPTA suppression (via negative feedback from increasing estradiol levels) that kicked in to drastically suppress testosterone levels 412/7.4 -> 16/1.4 -> 8/0.9. Thus, in summary, it appears that for this particular biologically male patient, mild HPTA suppression was beginning to exert negative feedback effects as estradiol levels rose to 43pg/mL and this HPTA suppression via negative feedback accelerated rapidly to almost complete suppression by the time estradiol levels had increased to
62pg/mL.
So what does this mean? Perhaps nothing, or perhaps this may point to a "biological set point" or "biological upper limit/ceiling" for estradiol levels in genetic males, after which profound HPTA suppression kicks in as a preventative/protective measure to prevent further increase. If this is the case, it would appear this “ceiling” or biological upper set-point for estradiol (when exposed to normal physiologic endocrine feedback mechanisms) would lie somewhere in the range of 43pg/mL – 62 pg/mL. However, with the HPTA suppression appearing to begin with estradiol levels in the 40's and the drastic/profound suppression evident with estradiol levels of 62 pg/mL, I would argue that the “set- point” or “biological ceiling” would seem to be somewhere between these two extremes, with an educated assumption based on these data and my own clinical experience of 50-55pg/mL. Further, it would be a sound argument to state that any estradiol levels that fall outside (above) the biological set point (wherever that may be) for HPTA suppression (which once again is ingrained into our endocrine system as a self-limiting protective mechanism) would classify as supra-physiologic (i.e. above the levels for which normal HPTA suppression in a male would PREVENT levels from rising).
There are limitations to this study including small sample size, not monitoring LH/FSH but instead relying on observed testosterone suppression as a surrogate measure of HPTA suppression, and lack of more precise measurement of estradiol levels, particularly during the interval of apparent HPTA suppression of 43pg/mL – 62pg/mL. Nonetheless, I feel that this data represents a unique and novel insight into what one might consider ‘physiologic” estradiol levels as measured by the endocrine system's own measuring stick – HPTA suppression via the evolutionary negative feedback mechanism.
Last edited by a moderator:
Vince Carter
Banned
Except for the formatting, her eit is, but the .pdf reader is a free download from Adobe.
Save for the real topic which I do find disagreeable, there's key info here for males in one of those unknown areas, what exactly is high Estradiol, there's never quite been a limit placed on that, like some hard and fast point that we could say you don't want to go higher than...in this case, 43. Up from 43 HPTA suppression begins and accelerates from there.
Save for the real topic which I do find disagreeable, there's key info here for males in one of those unknown areas, what exactly is high Estradiol, there's never quite been a limit placed on that, like some hard and fast point that we could say you don't want to go higher than...in this case, 43. Up from 43 HPTA suppression begins and accelerates from there.
Nelson Vergel
Founder, ExcelMale.com
Good article, Dr Saya. Very informative for men whose HPTA is not already suppressed. It reinforces the upper limit of E2 in men wit endogeneous testosterone production. But for men on TRT with fully suppressed HPTA, this information may not be applicable since they have artificially high T and no concerns about HPTA suppression since that is a given with TRT.
We know that in a healthy male about .3 % of T converts to E2. This means that E2 will go up as T increases. Nature and evolution have ensured that we have enough E2 to balance T. Why disrupt this balance with anastrozole unless the conversion is much above .3% due to liver, fat, or medication effects on aromatization?
We have very few data on T/E2 ratios and how they correlate to fertility, the best endpoint for proper HPTA function. Do we really need to improve a T/E2 ratio that is already over 14 with the use of anastrozole? I have not found a study that looks into that yet.
https://www.excelmale.com/forum/sho...tosterone-to-Estradiol-Ratio-Important-in-Men
We know that in a healthy male about .3 % of T converts to E2. This means that E2 will go up as T increases. Nature and evolution have ensured that we have enough E2 to balance T. Why disrupt this balance with anastrozole unless the conversion is much above .3% due to liver, fat, or medication effects on aromatization?
We have very few data on T/E2 ratios and how they correlate to fertility, the best endpoint for proper HPTA function. Do we really need to improve a T/E2 ratio that is already over 14 with the use of anastrozole? I have not found a study that looks into that yet.
https://www.excelmale.com/forum/sho...tosterone-to-Estradiol-Ratio-Important-in-Men
Dr Justin Saya MD
Moderator
I find it very interesting and intriguing to gain some insight into where the natural and intact male HPTA begins to "hit the brakes" when it comes to increasing estradiol levels...
Nelson Vergel
Founder, ExcelMale.com
I think this would make a great conference presentation
Dr Justin Saya MD
Moderator
I appreciate that and agree, Nelson. We'll chat about it privately.
Dr Justin Saya MD
Moderator
What is the possible mechanism that raising estradiol levels will increase testosterone production?
I can't seem to understand how that would even work.
I would stress that this is only an interesting observation at this point, but fun to think about nonetheless. If this were found to be true in a general sense (i.e. increasing estradiol levels from LOW range (12pg/mL) up into NORMAL range (12 -> 22pg/mL) resulted in HPTA stimulation and thus increased testosterone levels (I will need to repeat similar study with LH/FSH for better data), it could imply that the regulatory mechanisms of the HPTA are more complex than currently believed...both positive and negative feedback AND perhaps a concentration-dependent relationship determining whether the feedback is positive or negative (i.e. estradiol exerts positive feedback up to a certain point, after which negative feedback kicks in). Obviously just purely scientific speculation, but really fun to think about, isn't it?
I also want to be clear that I am NOT taking a position that giving estradiol to a male patient that presents with both low T and E may enhance testosterone levels...this was merely an intriguing and thought-provoking observation at this point. Treating a non-MTF male with estradiol would create the perfect environment for a no-defense slam dunk gynecomastia malpractice case and would likely give my malpractice carrier an aneurysm!
Lastly, even though I realize to some the "subject matter" of this study may be offensive, I urge everyone to keep an open mind and not allow personal judgment or prejudices to cloud the medical/scientific discussion. I personally am very grateful for the unique perspective into the function and physiology of sex hormones that treating a very selective group of MTF/FTM transgenders has given me. I feel it has broadened my understanding and expertise and, ultimately, made me a better physician for ALL of my patients.
Wow that was an interesting reply. I love the science behind hormones, and love thinking about different mechanisms that allow the endocrine system to function in my free time.
What you're describing sounds almost like a biphasic effect of estradiol in the feedback loop. I think that makes sense, as a layman of course. What about the possibility of down-regulation of estrogen receptors. possibly on the hypothalamus or pituitary? Less receptors, less effect = the body producing more testosterone in order to increase estradiol? From what I understand, testosterone itself also provides some of the negative feedback in the HPTA for men as well, I'm assuming that estradiol has a stronger effect than testosterone, right?
You're right this is incredibly interesting. I of course understand that you wouldn't support treating a low t and e male patient with estradiol.
If possible, how would you treat a male patient with normal testosterone(or low normal) and very low estradiol? Obviously if you can't give estradiol, the only way to fix that is testosterone? Keep in mind I am NOT taking this a diagnosis, or treatment, merely taking it as information.
I am considering using defy, but I am concerned that I will be told again that I can't be treated due to my levels being too high. 400-500 ng/dl total testosterone, but low estradiol. All of the doctors I have seen have told me they can't treat me due to my young age(25), and I don't want to waste anymore time or money in having doctors tell me they can't help. I am frustrated you know?
What you're describing sounds almost like a biphasic effect of estradiol in the feedback loop. I think that makes sense, as a layman of course. What about the possibility of down-regulation of estrogen receptors. possibly on the hypothalamus or pituitary? Less receptors, less effect = the body producing more testosterone in order to increase estradiol? From what I understand, testosterone itself also provides some of the negative feedback in the HPTA for men as well, I'm assuming that estradiol has a stronger effect than testosterone, right?
You're right this is incredibly interesting. I of course understand that you wouldn't support treating a low t and e male patient with estradiol.
If possible, how would you treat a male patient with normal testosterone(or low normal) and very low estradiol? Obviously if you can't give estradiol, the only way to fix that is testosterone? Keep in mind I am NOT taking this a diagnosis, or treatment, merely taking it as information.
I am considering using defy, but I am concerned that I will be told again that I can't be treated due to my levels being too high. 400-500 ng/dl total testosterone, but low estradiol. All of the doctors I have seen have told me they can't treat me due to my young age(25), and I don't want to waste anymore time or money in having doctors tell me they can't help. I am frustrated you know?
Last edited:
Dr Justin Saya MD
Moderator
Yes estradiol tends to show at least equivalent, if not stronger, suppression of the HPTA as testosterone.
DHEA may help you if your levels aren't already high-normal.
Most younger guys are more secondary/tertiary hypogonadal (relatively low LH/FSH) and, if you fall into this category, Clomid would be a great option for you with regards to your age and your low estradiol levels.
DHEA may help you if your levels aren't already high-normal.
Most younger guys are more secondary/tertiary hypogonadal (relatively low LH/FSH) and, if you fall into this category, Clomid would be a great option for you with regards to your age and your low estradiol levels.
Well it seems that you would treat me even though I am young. I already have high dhea. Also have high LH, from what I've read, the target with clomid is to get LH to about 7-8 on a 1.6-8.6 range right? I'm already there, which is why I guess most doctors don't want to treat me, that leaves the only option as testosterone. Could clomid still be a possibility? I would love to do that instead.
Dr Justin Saya MD
Moderator
Well it seems that you would treat me even though I am young. I already have high dhea. Also have high LH, from what I've read, the target with clomid is to get LH to about 7-8 on a 1.6-8.6 range right? I'm already there, which is why I guess most doctors don't want to treat me, that leaves the only option as testosterone. Could clomid still be a possibility? I would love to do that instead.
Clomid may still offer some benefit at your age...LH levels are often capable of safely going quite a bit higher than 7-8, although that does hint at more of a primary hypogonadal picture. HCG monotherapy would be another consideration. Either one would also serve as a DIAGNOSTIC treatment to accurately determine if, and to what degree, you are primary hypogonadal (in which case TRT would then be your most suitable option if symptoms dictated).
Dr Justin Saya MD
Moderator
Thank you, I hate to question you so much. It's just that with how many doctors I've seen and how many doctors dismissed my symptoms it's hard to just trust that I'm not wasting time and money.
I never knew that LH can safely go higher than 7-8, so more like 11 or higher?
In a young guy such as yourself, yes...and THAT would conclusively determine if your testes are capable of producing adequate testosterone levels (i.e. if you are primary or not).
DragonBits
Well-Known Member
Attached a case study just wrapped up that may be of interest to some of you!
Will also try to paste plain text below for those that cannot open pdf.
Very interesting data old thread from Dr. Saya, implies that E2 should be at least 20-30 pg/ml in most men.
Though I am not sure about the balance part. Meaning if you have very high TT/FT, and ~3% is E2, does that high E2 have a negative effect.
Last edited:
Vince
Super Moderator
My LH was 14 before I started TRT.Thank you, I hate to question you so much. It's just that with how many doctors I've seen and how many doctors dismissed my symptoms it's hard to just trust that I'm not wasting time and money.
I never knew that LH can safely go higher than 7-8, so more like 11 or higher?
joshmaximus
Member
What is normal estradiol levels? Where do u like to see your patient at? No higher than what?Yes estradiol tends to show at least equivalent, if not stronger, suppression of the HPTA as testosterone.
DHEA may help you if your levels aren't already high-normal.
Most younger guys are more secondary/tertiary hypogonadal (relatively low LH/FSH) and, if you fall into this category, Clomid would be a great option for you with regards to your age and your low estradiol levels.
Online statistics
- Members online
- 6
- Guests online
- 5
- Total visitors
- 11
Totals may include hidden visitors.
© Copyright 2020 ExcelMale
















