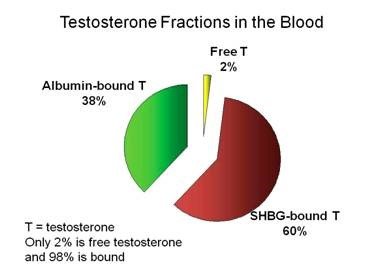
what is the typical % ranges for SHBG and albumin in regards to testosterone fractions in the blood?
The image is one examaple but Every source I come accross says a different thing. We know that 98% is bound. 2% is free... of course the amount bound (SHBG/albumin) is going to be user specific dependent on many factors....but what would be typical % range for the average healthy man?
some sources say 45% SHBG and 53-55% albumin. Others have SHBG as high as 60-70% so what’s typical...
@Nelson Vergel
Many thanks.
The image is one examaple but Every source I come accross says a different thing. We know that 98% is bound. 2% is free... of course the amount bound (SHBG/albumin) is going to be user specific dependent on many factors....but what would be typical % range for the average healthy man?
some sources say 45% SHBG and 53-55% albumin. Others have SHBG as high as 60-70% so what’s typical...
@Nelson Vergel
Many thanks.