madman
Super Moderator
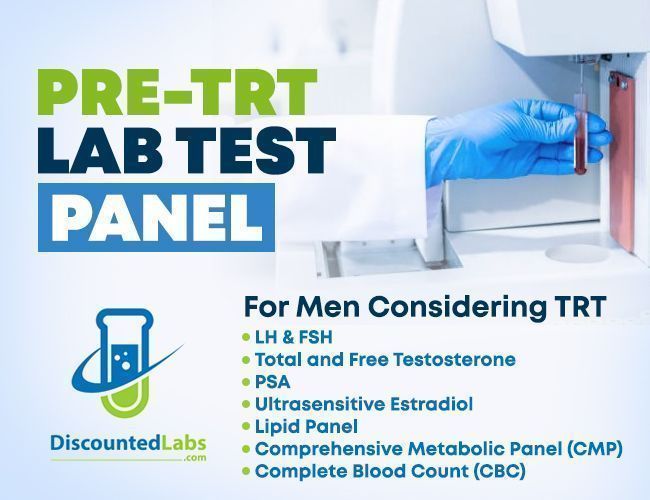
Click here for:
PRE-TRT LAB TESTS
The Pre-Testosterone Therapy Checklist (2022)
Jose M. Flores, MD, MHA, and John P. Mulhall, MD, MSc, FECSM, FACS, FRCSI
INTRODUCTION
In contemporary practice, there are a myriad of testosterone therapy (TTH) modalities of exogenous TTH in the form of oral agents, gels, patches, transnasal agents, and subcutaneous and intramuscular injections. A number of so-called alternative agents are available to patients, especially those for whom fertility is a major concern, in the form of clomiphene citrate, aromatase inhibitors, and human chorionic gonadotropin.
The AUA guidelines on Testosterone (T) deficiency and TTH (2018), in men with low T (2 morning total T levels ≤ 300 ng/dL) before TTH, recommend evaluating these men for (i) the presence of breast symptoms of gynecomastia, (ii) their interest in fertility, (iii) a baseline hematocrit, (iv) and a PSA level in men over 40 years of age.1,2 The European Association of Urology guidelines on male hypogonadism (2020) recommend a similar assessment in such men adding, (v) the history of bone density loss.2,3 However, there is no guidance as to how an individual practitioner should define which modality is optimal for any given individual patient. Furthermore, a number of conditions warrant further investigation and should cause the practitioner to pause prior to writing a TTH prescription.
For some years now, we have used a TTH checklist to give patients guidance regarding the optimal mode of therapy and to guide prescribers as to whether a further patient evaluation is warranted. Such checklists are useful in promoting consistency of decision-making across a team in an effort to optimize patient safety and satisfaction. In our experience, the cost to the patient and individual patient preference are key initial factors in determining which modality patients will choose. However, factors such as baseline PSA and hematocrit level, prostate considerations, risk of transference, interest in fertility, cardiovascular event history, use of anticoagulant medication, and presence of breast symptoms or gynecomastia are important considerations in deciding whether to initiate TTH as well as defining the optimal therapeutic modality.
Patient Preference for Testosterone Therapy Modality
The AUA guidelines advise physicians to take into account patient preferences before starting TTH.1 Identifying patient preferences is critical to improving adherence and compliance with the treatment.4 Contradictory reports have been published regarding patient preference. For example, one study reported that more than half of patients chose injections followed by T gel, however, in this report, these choices were significantly related to the lower price of injection therapy.5 However, in another study that compared the preference for transdermal gel against injection, 79% preferred transdermal TTH due to convenience, ease of use, and not having to go to a physician’s office to receive injections, and pain avoidance.6 Our initial objective is to identify the patient’s preference without other factors influencing their decision.
Cost
In much of the world, TTH is not a covered prescription benefit. In some parts of the world, some modalities are covered. In our clinical practice, we provide a TTH medication list to patients that present all brand and generic TTH options and we suggest to the patient that he explore the cost of therapy. Setting realistic expectations for patients with regard to long-term costs is a valuable early step in managing a TTH program.
Baseline Hematocrit Level
Guidelines recommend measuring a hematocrit level before commencing TTH. If this level is elevated >50%, an investigation should occur to define the etiology of this elevation, which includes hematological issues, obstructive sleep apnea (OSA), pulmonary disease, or patients living at elevation. It is well known that TTH can be associated with elevation of hematocrit and possibly polycythemia resulting from an increase in erythropoietic activity. It has been reported that men with OSA have double the risk of polycythemia, compared to men without OSA after starting TTH (20% vs 10%).7 Polycythemia is associated with potentially serious consequences such as venothromboembolic events (VTE), myocardial infarction, and stroke.8 Given the association between TTH and polycythemia, men with TD in our practice are screened for OSA using validated questionnaires. A STOP-BANG score ≥3 has a sensitivity/specificity to diagnosis OSA of 87%/30% respectively.9 If these questionnaires suggest a patient is at moderate-high risk of OSA they are encouraged to undergo a home sleep apnea test prior to commencing TTH.
Baseline PSA Level
Guidelines recommend assessing patients prior to TTH for a history of prostate cancer and measuring a baseline PSA level in men over 40 years of age.1 As part of shared decision-making, such patients have a PSA level at baseline and if abnormal undergo further testing prior to TTH is started. Several studies have reported a prevalence of prostate cancer in men with low T between 15% and 30%.10−12 It is worth noting that Morgentaler in 1999 showed that 14% of men with TD and a PSA ≤4 ng/mL had a prostate biopsy-proven prostate cancer.12 Low testosterone levels have also been associated with a higher high Gleason score in men with concomitant prostate cancer.13,14 Although the label for TTH states that TTH is contraindicated in men with prostate cancer, the contemporary practice has questioned such an approach, and an accumulation of data suggests that at least in men with organ-confined, low-intermediate prostate cancer TTH can be considered. This is supported by the 2018 AUA TD guidelines.1
Transference Risk
Guidelines recommend discussing the risk of transmitting exogenous T to children and women from men using transdermal TTH (transference, TF).1 Indeed, there is a black box warning for this in the USA. TF can lead to hyperandrogenism with virilization in women and precocious puberty in children. We ask all patients regarding contact with prepubertal boys as well as females of any age plus, as well the frequency of such contact. Every candidate for transdermal TTH is assigned a low TF risk, given the chance of inadvertent contact with children. However, all men with regular contact with10 pre-pubertal boys or girls are considered at high risk of TF, and in this group of patients, we decline to prescribe transdermal TTH. The greatest TF risk is through direct skin-to-skin contact, 60% of applied T can be recovered directly from unwashed skin 8 hours after application, and 14% if the skin has been washed.15 A single study has demonstrated that up to 13% of the dose applied to the axilla can be recovered from unwashed clothing, and after laundering, up to 3% of the dose remains. It is also worth noting that after laundering the clothing, approximately 6% of the T dose was also found on other clothes.16 Patients must always be reminded to wash their hands thoroughly after gel/cream application. Patients and their families are often not aware of this risk of TF and fail to take precautions to reduce it, despite a clear warning on the label of these products. Potential legal repercussions have resulted from the failure of clinicians to document this conversation in the patient’s medical record.
Fertility Interest
A reproductive health evaluation is recommended before TTH is commenced if the patient with TD is interested infertility.1 To evaluate the patient’s current and future interest infertility. It is our experience that most patients are unaware of the impact of exogenous TTH on spermatogenesis. Contraception studies have shown that approximately 70% of the men become azoospermic within 6 months of commencing TTH and while 84% of men recover a sperm concentration of ≥20 million/mL 4 months after cessation of TTH, only half return to pre-treatment sperm concentration levels17,18 it is important to understand that these contraception studies were performed in young men without TD, using exogenous TTH for a period of 12 months, and caution must be exercised in extrapolating the spermatogenesis recovery data to the TD population, especially those men using TTH for periods longer than 1 year. Just as with transference risk, documentation of the patient’s reproductive interest should be recorded in the medical record. For such patients, we utilize clomiphene citrate (CC), hCG or aromatase inhibitors (AI), where appropriate.
Baseline LH Level
Guidelines recommend assessing an LH level among males with low T1 to define the type of hypogonadism in an effort to define the need for pituitary/hypothalamus imaging and to establish a baseline level before starting TTH or alternative treatments (CC, hCG, AI). A serum LH level can also help guide clinical decision-making in the evaluation of the patient’s candidacy for these alternative therapies. Prior studies have suggested that the ability to achieve therapeutic T levels decreases with increasing baseline LH levels.19,20 In men using CC, the on-treatment LH level will inform the clinician as to whether the pituitary is responsive (increase in LH level on CC) or not (no or minimal increase in LH level). For the patient whose LH level does not rise on CC, a dose increase will not make any difference in T level, while men with an increased LH level but with a less than satisfactory increase in serum T may benefit from a CC dose increase.
Prolactin Level
Guidelines recommend assessing prolactin levels before commencing TTH in men with low T levels combined with low or low/normal LH so as not to miss the co-existence of a pituitary lesion (such as a prolactinoma).1 Prolactinoma is still considered a rare disease with a prevalence of 75−115 cases per 100,000 per year, however, failing to diagnose one may result in missing a potential space-occupying lesion (optic chiasm compression and the risk of bitemporal hemianopsia) or the possibility of managing the patient using medications to reduce serum prolactin level without the need for formal TTH (bromocriptine, cabergoline).21 For men with low serum T with low/low normal LH levels, we obtain a prolactin level and if persistently elevated, a pituitary MRI is performed.
Anticoagulant Medications
Anticoagulant medications (ACM) are not mentioned in any guidelines, however, we suggest all patients on ACM exploring subcutaneous (SC) or intramuscular (IM) TTH injections should be counseled about bleeding issues and hematoma formation. It is estimated the incidence of hematoma is up to 2% after minor procedures in men on ACM.22 In patients using SC or IM TTH we strongly suggest patients consider using noninjectable modalities. We decline to use implantable T pellets in men using ACM. In our practice, acetylsalicylic acid (ASA), irrespective of the dose is not considered a contraindication to injectable/implantable therapies.
Risk of Venothromboembolic Events (VTE)
In 2014, the FDA in the USA changed the label for T products, with a black-box warning for the development of VTE. However, systematic reviews generated for guidelines documents have failed to show such a link.1 Saying this, all patients should be questioned regarding prior VTE events. Men with a history of VTE while using TTH are counseled they may need additional evaluation, including clearance by a hematologist, before receiving a TTH prescription from us. Men with prior VTE off any form of TTH undergo a review of their prior hematology records and may need hematology clearance. While on TTH, a hematocrit level is measured at least every 6 months.
History of Cardiovascular Events
The AUA guideline panel, which included a cardiologist, definitively stated that men with TD should be counseled that TD is associated with an increased risk of MACE (myocardial infarction, stroke, and cardiovascular-related mortality). At this time, there is no definitive evidence linking TTH to an increase or a decrease in these cardiovascular events.1,23 Excluding 4 papers 24−27 all the remaining literature is either neutral or suggests a lower risk of MACE in TTH users. It is believed by many experts that these 4 papers are methodologically flawed and that they should not impact our decision-making in this regard. The AUA guideline encourages TTH prescribers to routinely document a comprehensive CV history on all TTH candidates, including information on prior myocardial infarction, cerebrovascular accident, congestive heart failure, or uncontrolled hypertension. Based solely on expert opinion (as it was an inclusion criterion for prior TTH trials), guidelines recommend that TTH be postponed for a period of 3−6 months in men who have had a recent cardiovascular event.
History of Breast Cancer/Gynecomastia
T product labels also state that breast cancer is a contraindication to TTH, given the aromatization of T to estrogens. Prior to TTH, patients should be questioned regarding the presence of any breast symptoms including breast or nipple tenderness, and nipple discharge, and should be examined to define if pre-existing gynecomastia exists. Gynecomastia is a risk factor for breast cancer, with up to 3% of men with gynecomastia developing breast cancer, and in those men with a family history of breast cancer, this prevalence rises to 7%.28 If gynecomastia is confirmed, we instruct the patient to schedule a mammogram (with or without ultrasound) to define the nature of the breast tissue. One study reported that approximately half of the men who complain of breast symptoms/gynecomastia after TTH had pre-existing gynecomastia.29 Another report reported that approximately 3% of men attending a men’s health clinic for sexual dysfunction had gynecomastia, and one-third of them had low testosterone.30 Once again, clear documentation of a normal breast exam is an important step for clinicians prior to commencing TTH.
SUMMARY
A pre-T therapy checklist is a systematic listing of factors/conditions that should be assessed prior to commencing TTH. Running through this list will aid in defining if further evaluation is required for the TD patient prior to starting TTH and may aid in defining which TTH modality is optimal for the patient. This checklist will go some way to protecting the prescribing clinician in the increasingly fraught TTH medico-legal environment.
Attachments
Last edited by a moderator: