madman
Super Moderator
Abstract
Prostate MRI has seen rapid growth in use in recent years as an advanced diagnostic modality to detect focal areas of clinically significant prostate cancer, identify an area for targeted biopsy, and guide management and surveillance. The increase in use has also led to increased diagnosis of incidental lesions arising from structures around the prostate. These incidental findings may be related to the genitourinary system or non- genitourinary system and may have a benign etiology that needs no additional follow-up, or it may require surveillance and management. The field of view in a multiparametric prostate MRI includes other pelvic organs, neurovascular bundles, bowel, lymph nodes, and bones. Being familiar with standard MRI characteristics and sound knowledge of the anatomy of the prostate and surrounding structures can help in distinguishing normal anatomy from pathology. Given that patients undertaking a prostate MRI are usually a cohort with increased anxiety from their known or suspicion of prostate cancer, it is important that radiologists are familiar with these common incidental findings to minimize anxiety to the patient, have a well-informed discussion with the referring clinician and reduce costs associated with unnecessary further testing and follow-up of benign incidental findings. Additionally, being able to diagnose more serious incidental pathologies early can be life-saving and potentially significantly alter patient management.
Introduction
Multiparametric MRI (mpMRI) prostate allows accurate anatomical and functional imaging of the prostate gland and diagnosis of significant (intermediate and high risk) prostate cancer [1]. mpMRI can also be utilized in active surveillance for patients with low- and intermediate-risk prostate cancer and guide targeted prostate biopsies.
Transrectal ultrasound (TRUS) and positron emission tomography (PET) are other imaging modalities which can be used to assess the prostate and aid in diagnosis and localization, therapy, staging, active surveillance and recurrence monitoring [2]. On TRUS, a relatively safe and inexpensive imaging modality, prostate cancer is most often hypoechoic relative to the normal peripheral zone but may sometimes be isoechoic or even hyperechoic. Further features that increase confidence in diagnosing prostate cancer on TRUS are asymmetry in prostate size (particularly in the peripheral zone), capsular distortion and loss of differentiation between the central gland and peripheral zone [2].
mpMRI of the prostate typically combines the anatomical images of T1- and T2-weighted imaging with functional sequences including diffusion-weighted imaging (DWI) (with a calculated b value of 2000), in conjunction with the apparent diffusion coefficient (ADC), and dynamic contrast enhancement (DCE) T1 sequences (using gadolinium-based IV contrast agents) [1, 3]. Te T2 sequence provides the best assessment of prostate margins for an extracapsular extension, seminal vesicle invasion, neurovascular bundle, and adjacent organ involvement [3]. T1 weighted imaging helps differentiate post-biopsy hemorrhage from the tumor [3]. DWI is useful because prostate cancer has a reduced diffusion of water, compared with normal prostate, due to its tightly packed cells [1, 3]. DCE imaging provides further functional information as malignancy causes changes such as increased blood flow, neo-vascularity, and leaky capillaries [1, 3]. Finally, magnetic resonance spectroscopy is a functional technique that indirectly measures metabolite levels of choline, creatinine, and citrate in the prostate but, due to being technically challenging and time-consuming, is often not included in a mpMRI protocol [1, 3].
The Prostate Imaging Reporting and Data system (PIRADS) is a structured reporting system allowing a weighted calculation on a 5-point scale and is based on the probability that a combination of the mpMRI parameters correlates with the presence of a clinically significant cancer [4]. An alternative method of reporting prostate MRI is using the five-point Likert scale where scores indicating higher suspicion (Likert 4–5) on MRI correlate strongly with a higher likelihood of overall cancer where a targeted biopsy might be useful [5].
In a prostate MRI, the field of view includes several key structures. Anterior relations of the prostate are pubic
symphysis and the retropubic space of Retzius. Posterior to the prostate is the rectovesical fascia and rectum. The bladder is superior to the prostate, and the urogenital membrane lies inferior to the prostate. The posterior wall of the bladder contacts the seminal vesicles, ampulla of the vas deferens, and the bladder venous plexus [6]. Seminal vesicles are located above and posterior to the prostate base. The prostatic neurovascular bundle (NVB) is situated laterally in the posterolateral angles of the prostate at 5 and 7 o’clock positions and gives branches into the prostate at the apex and base [6].
For a radiologist reviewing or reporting a mpMRI prostate, it is crucial that they are familiar with the imaging findings related to prostate cancer, but they must also have an understanding of incidental findings in the field of view, which may be indolent or has a significant impact on the patient’s management.
Recent studies have found incidental findings in the range of 42% [7]–52.7% [8]. While the majority of true incidental findings were non-urological, 6.6% of these were considered clinically significant [7]. Incidental findings were noted to be more common in patients aged over 65, with a ratio of 57% versus 46% in patients aged under 65 [8]. 4.2% of patients required surgery for incidental findings including bladder cancer (1.1%), testicular tumor (0.5%), and rectal cancer (0.3%) [8], further affirming the importance of detection and interpretation of incidental findings early.
The purpose of this pictorial review is to illustrate some common incidental findings, as classified by systems and outlined in Table 1, that the radiologist may encounter when reporting a prostate MRI. These incidental findings can have clinically significant as well as indolent outcomes, and early and accurate identification can alter management. Being familiar with the anatomy of the prostate and peri-prostatic spaces and pertinent MR signal characteristics can help formulate differential diagnoses for an incidental finding while the patient’s age, clinical history and recent interventions, if any, can help further, narrow the differential list.
Our case selection depicts the spectrum of cases encountered in daily practice in a tertiary referral center over the past five years in patients’ having prostate MRI is influenced by the demographics and history of the patients referred to our department. We highlight some cases of incidental findings that can be seen in spaces and structures around the prostate classified by systems in Table 1, as well as within the prostate and the periprostatic region which is further outlined in Table 2.
Prostate and periprostatic region
Haematospermia with and without a stone in seminal vesicles
Prostate calcification
Prostatic utricle cyst
Mullerian duct cyst
Cowper’s gland duct cyst
Periprostatic hematoma post‑biopsy
Prostate TB abscess in a patient with bladder TCC after intravesical instillation of BCG
Periprostatic dermoid cyst
Prostate adenocarcinoma with a large right seminal vesicular cyst
Musculoskeletal
Periprostatic leiomyoma
Periprostatic leiomyosarcoma
Solitary fibrous tumor
Lipoma and liposarcoma
Parachordoma (also known as myoepithelial carcinoma)
Urological
Bladder wall thickening and hydrocele
Undifferentiated pleomorphic sarcoma (UPS) of the spermatic cord
Spermatic cord lymphoma
Urothelial carcinoma
Colorectal
Inguinal hernia
Ascites
Rectal Gastrointestinal Stromal Tumours (GIST)
Rectal villous adenomas
Rectal adenocarcinoma
Vascular
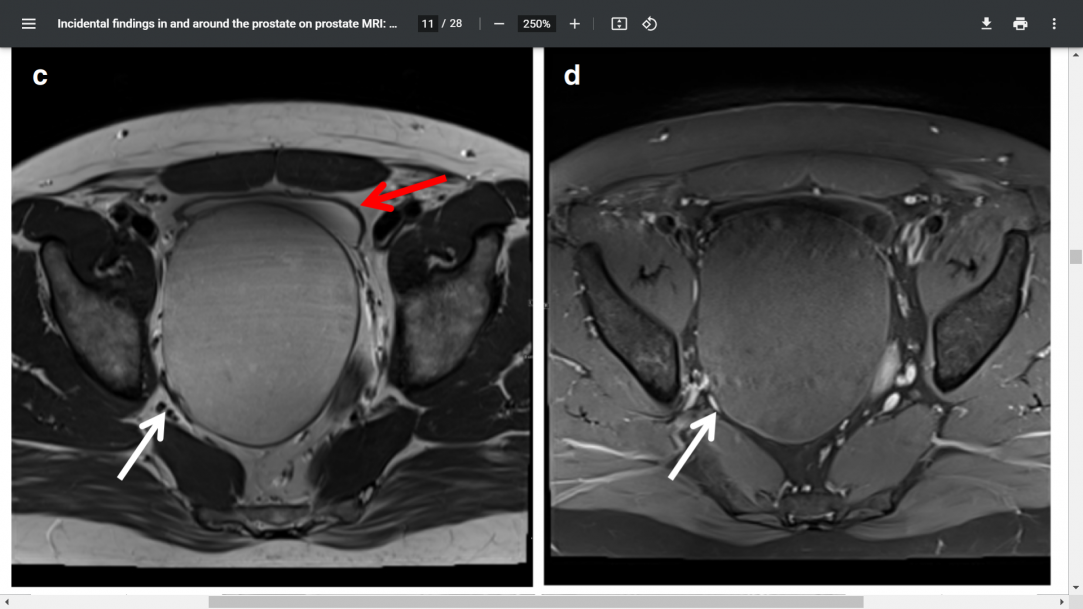
Periprostatic venous varix
Lymphadenopathy
Conclusion
Prostate MRI continues to expand in its utility in the diagnosis, management, and surveillance of prostate cancer. It allows detection of both clinically significant and indolent incidental findings in the field of view including abdominal and pelvic organs, vessel and bones. There are a myriad of lesions that can either arise from or be in the vicinity of the prostate that can be missed or incorrectly diagnosed by the radiologist not familiar with reporting prostate MRI commonly.
A systemic approach with a review of the distal ureters, bladder, and rectum as check areas, is important as several incidental findings in these locations can be neoplastic. Sound knowledge of the anatomical structures in the field of view will help guide towards the origin of the lesion and assist in characterizing as some locations are characteristic such as the prostatic venous plexus around the posterolateral aspect of the prostate gland. Localizing the pathology to an organ significantly helps in narrowing the differential list. Some MRI signal characteristics of hemorrhage and calcification are important to recognize as they provide important clues for the differential diagnosis. Being aware of the clinical backgrounds such as recent intervention or haematuria in the case of hemorrhage, or history of intravesical BCG for TCC in the case of a prostatic abscess, can greatly contribute to increased confidence in making a diagnosis. Often leiomyomas and benign mesenchymal tumors can be difficult to differentiate based on imaging alone and a biopsy for histological and immunohistochemistry may be inevitable to confirm the pathology.
When identifying a cystic structure, the main considerations should be between a utricle cyst and a Mullerian duct cyst. The former is typically smaller, midline, and does not extend above the base of the prostate. When identifying a solid lesion assess for the presence of blood products or fat as these can narrow the differential. Once the presence of a solid mass separate from the prostate is established, it can be challenging to differentiate benign and malignant soft tissue tumors, and often a targeted biopsy is required. However, being able to recognize common lesion characteristics, in conjunction with patient demographics and background, helps reach a succinct and accurate list of differential diagnoses.
It is important for the reporting radiologist to be aware that these exist to be able to make an adequate assessment and also that although they may be benign or malignant, their detection and follow-up often has implications on clinical management, patient anxiety and increased cost. This is especially important given that prostate MRI is often performed for patients that have known or strong suspicion and risk for prostate cancer and is already a cohort with significant stressors and anxiety. Hence, it is prudent that radiologists are able to develop skills in diagnosing these lesions and collaborating with the referrer on a management plan.
Prostate MRI has seen rapid growth in use in recent years as an advanced diagnostic modality to detect focal areas of clinically significant prostate cancer, identify an area for targeted biopsy, and guide management and surveillance. The increase in use has also led to increased diagnosis of incidental lesions arising from structures around the prostate. These incidental findings may be related to the genitourinary system or non- genitourinary system and may have a benign etiology that needs no additional follow-up, or it may require surveillance and management. The field of view in a multiparametric prostate MRI includes other pelvic organs, neurovascular bundles, bowel, lymph nodes, and bones. Being familiar with standard MRI characteristics and sound knowledge of the anatomy of the prostate and surrounding structures can help in distinguishing normal anatomy from pathology. Given that patients undertaking a prostate MRI are usually a cohort with increased anxiety from their known or suspicion of prostate cancer, it is important that radiologists are familiar with these common incidental findings to minimize anxiety to the patient, have a well-informed discussion with the referring clinician and reduce costs associated with unnecessary further testing and follow-up of benign incidental findings. Additionally, being able to diagnose more serious incidental pathologies early can be life-saving and potentially significantly alter patient management.
Introduction
Multiparametric MRI (mpMRI) prostate allows accurate anatomical and functional imaging of the prostate gland and diagnosis of significant (intermediate and high risk) prostate cancer [1]. mpMRI can also be utilized in active surveillance for patients with low- and intermediate-risk prostate cancer and guide targeted prostate biopsies.
Transrectal ultrasound (TRUS) and positron emission tomography (PET) are other imaging modalities which can be used to assess the prostate and aid in diagnosis and localization, therapy, staging, active surveillance and recurrence monitoring [2]. On TRUS, a relatively safe and inexpensive imaging modality, prostate cancer is most often hypoechoic relative to the normal peripheral zone but may sometimes be isoechoic or even hyperechoic. Further features that increase confidence in diagnosing prostate cancer on TRUS are asymmetry in prostate size (particularly in the peripheral zone), capsular distortion and loss of differentiation between the central gland and peripheral zone [2].
mpMRI of the prostate typically combines the anatomical images of T1- and T2-weighted imaging with functional sequences including diffusion-weighted imaging (DWI) (with a calculated b value of 2000), in conjunction with the apparent diffusion coefficient (ADC), and dynamic contrast enhancement (DCE) T1 sequences (using gadolinium-based IV contrast agents) [1, 3]. Te T2 sequence provides the best assessment of prostate margins for an extracapsular extension, seminal vesicle invasion, neurovascular bundle, and adjacent organ involvement [3]. T1 weighted imaging helps differentiate post-biopsy hemorrhage from the tumor [3]. DWI is useful because prostate cancer has a reduced diffusion of water, compared with normal prostate, due to its tightly packed cells [1, 3]. DCE imaging provides further functional information as malignancy causes changes such as increased blood flow, neo-vascularity, and leaky capillaries [1, 3]. Finally, magnetic resonance spectroscopy is a functional technique that indirectly measures metabolite levels of choline, creatinine, and citrate in the prostate but, due to being technically challenging and time-consuming, is often not included in a mpMRI protocol [1, 3].
The Prostate Imaging Reporting and Data system (PIRADS) is a structured reporting system allowing a weighted calculation on a 5-point scale and is based on the probability that a combination of the mpMRI parameters correlates with the presence of a clinically significant cancer [4]. An alternative method of reporting prostate MRI is using the five-point Likert scale where scores indicating higher suspicion (Likert 4–5) on MRI correlate strongly with a higher likelihood of overall cancer where a targeted biopsy might be useful [5].
In a prostate MRI, the field of view includes several key structures. Anterior relations of the prostate are pubic
symphysis and the retropubic space of Retzius. Posterior to the prostate is the rectovesical fascia and rectum. The bladder is superior to the prostate, and the urogenital membrane lies inferior to the prostate. The posterior wall of the bladder contacts the seminal vesicles, ampulla of the vas deferens, and the bladder venous plexus [6]. Seminal vesicles are located above and posterior to the prostate base. The prostatic neurovascular bundle (NVB) is situated laterally in the posterolateral angles of the prostate at 5 and 7 o’clock positions and gives branches into the prostate at the apex and base [6].
For a radiologist reviewing or reporting a mpMRI prostate, it is crucial that they are familiar with the imaging findings related to prostate cancer, but they must also have an understanding of incidental findings in the field of view, which may be indolent or has a significant impact on the patient’s management.
Recent studies have found incidental findings in the range of 42% [7]–52.7% [8]. While the majority of true incidental findings were non-urological, 6.6% of these were considered clinically significant [7]. Incidental findings were noted to be more common in patients aged over 65, with a ratio of 57% versus 46% in patients aged under 65 [8]. 4.2% of patients required surgery for incidental findings including bladder cancer (1.1%), testicular tumor (0.5%), and rectal cancer (0.3%) [8], further affirming the importance of detection and interpretation of incidental findings early.
The purpose of this pictorial review is to illustrate some common incidental findings, as classified by systems and outlined in Table 1, that the radiologist may encounter when reporting a prostate MRI. These incidental findings can have clinically significant as well as indolent outcomes, and early and accurate identification can alter management. Being familiar with the anatomy of the prostate and peri-prostatic spaces and pertinent MR signal characteristics can help formulate differential diagnoses for an incidental finding while the patient’s age, clinical history and recent interventions, if any, can help further, narrow the differential list.
Our case selection depicts the spectrum of cases encountered in daily practice in a tertiary referral center over the past five years in patients’ having prostate MRI is influenced by the demographics and history of the patients referred to our department. We highlight some cases of incidental findings that can be seen in spaces and structures around the prostate classified by systems in Table 1, as well as within the prostate and the periprostatic region which is further outlined in Table 2.
Prostate and periprostatic region
Haematospermia with and without a stone in seminal vesicles
Prostate calcification
Prostatic utricle cyst
Mullerian duct cyst
Cowper’s gland duct cyst
Periprostatic hematoma post‑biopsy
Prostate TB abscess in a patient with bladder TCC after intravesical instillation of BCG
Periprostatic dermoid cyst
Prostate adenocarcinoma with a large right seminal vesicular cyst
Musculoskeletal
Periprostatic leiomyoma
Periprostatic leiomyosarcoma
Solitary fibrous tumor
Lipoma and liposarcoma
Parachordoma (also known as myoepithelial carcinoma)
Urological
Bladder wall thickening and hydrocele
Undifferentiated pleomorphic sarcoma (UPS) of the spermatic cord
Spermatic cord lymphoma
Urothelial carcinoma
Colorectal
Inguinal hernia
Ascites
Rectal Gastrointestinal Stromal Tumours (GIST)
Rectal villous adenomas
Rectal adenocarcinoma
Vascular
Periprostatic venous varix
Lymphadenopathy
Conclusion
Prostate MRI continues to expand in its utility in the diagnosis, management, and surveillance of prostate cancer. It allows detection of both clinically significant and indolent incidental findings in the field of view including abdominal and pelvic organs, vessel and bones. There are a myriad of lesions that can either arise from or be in the vicinity of the prostate that can be missed or incorrectly diagnosed by the radiologist not familiar with reporting prostate MRI commonly.
A systemic approach with a review of the distal ureters, bladder, and rectum as check areas, is important as several incidental findings in these locations can be neoplastic. Sound knowledge of the anatomical structures in the field of view will help guide towards the origin of the lesion and assist in characterizing as some locations are characteristic such as the prostatic venous plexus around the posterolateral aspect of the prostate gland. Localizing the pathology to an organ significantly helps in narrowing the differential list. Some MRI signal characteristics of hemorrhage and calcification are important to recognize as they provide important clues for the differential diagnosis. Being aware of the clinical backgrounds such as recent intervention or haematuria in the case of hemorrhage, or history of intravesical BCG for TCC in the case of a prostatic abscess, can greatly contribute to increased confidence in making a diagnosis. Often leiomyomas and benign mesenchymal tumors can be difficult to differentiate based on imaging alone and a biopsy for histological and immunohistochemistry may be inevitable to confirm the pathology.
When identifying a cystic structure, the main considerations should be between a utricle cyst and a Mullerian duct cyst. The former is typically smaller, midline, and does not extend above the base of the prostate. When identifying a solid lesion assess for the presence of blood products or fat as these can narrow the differential. Once the presence of a solid mass separate from the prostate is established, it can be challenging to differentiate benign and malignant soft tissue tumors, and often a targeted biopsy is required. However, being able to recognize common lesion characteristics, in conjunction with patient demographics and background, helps reach a succinct and accurate list of differential diagnoses.
It is important for the reporting radiologist to be aware that these exist to be able to make an adequate assessment and also that although they may be benign or malignant, their detection and follow-up often has implications on clinical management, patient anxiety and increased cost. This is especially important given that prostate MRI is often performed for patients that have known or strong suspicion and risk for prostate cancer and is already a cohort with significant stressors and anxiety. Hence, it is prudent that radiologists are able to develop skills in diagnosing these lesions and collaborating with the referrer on a management plan.
Attachments
Last edited: